Estimated Reading Time: 18-20 minutes (3,706 words)
Introduction
Healthcare is evolving at lightning speed, and one of the most transformative innovations of the last decade is Remote Patient Monitoring (RPM). Imagine a world where patients with chronic illnesses—diabetes, hypertension, heart disease, or COPD—can be continuously monitored from the comfort of their homes, while doctors receive real-time data to intervene before emergencies arise. This isn’t science fiction; it’s happening today, globally and in India.
RPM is not just about convenience—it’s saving lives. By detecting early warning signs, preventing hospital readmissions, and improving chronic-disease management, RPM is reshaping the way healthcare is delivered. For countries like India, where hospital resources are stretched and chronic disease prevalence is rising, RPM provides a scalable, cost-effective solution that can reach urban and rural populations alike.
In this blog, we will explore how RPM works, the technologies driving it, real-world evidence of its life-saving impact, market trends in India and worldwide, and what the next 10 years hold for this revolutionary healthcare tool. Whether you are a healthcare professional, policymaker, or patient, understanding RPM today could help you prepare for the future of health tomorrow.
What is Remote Patient Monitoring (RPM)?
Remote Patient Monitoring (RPM) is a cutting-edge healthcare approach that leverages digital technologies, connected devices, and telemedicine platforms to monitor patients’ health outside traditional clinical settings. This includes homes, rural or remote locations, and post-discharge recovery periods. Rather than relying solely on periodic hospital visits, RPM allows for continuous health oversight, giving doctors real-time data to make timely interventions. (Wikipedia)
How RPM Works
RPM systems typically involve wearables, vital-sign monitors, and mobile or IoT-enabled devices that track key health metrics such as:
- Blood pressure (BP)
- Blood glucose levels
- Heart rate and ECG patterns
- Oxygen saturation (SpO₂)
- Weight, temperature, and other patient-reported symptoms
These measurements are transmitted securely to healthcare providers via cloud-based platforms or telemedicine apps. Advanced RPM platforms may include AI-driven analytics that detect anomalies, flag potential emergencies, and provide actionable insights to care teams.
Integration with Broader Care Models
RPM is often part of virtual wards or “hospital-at-home” programs, where patients receive hospital-level monitoring and interventions while remaining at home. For instance:
- Heart failure patients may have wearable monitors that transmit daily weight and blood pressure data; alerts are triggered if readings indicate fluid retention, prompting early clinical intervention.
- Diabetic patients can use continuous glucose monitors (CGM) that sync with apps, alerting care teams if blood sugar levels spike or drop dangerously.
These models not only enhance patient convenience but also reduce hospital overcrowding, especially critical in countries like India with high population density and limited hospital resources.
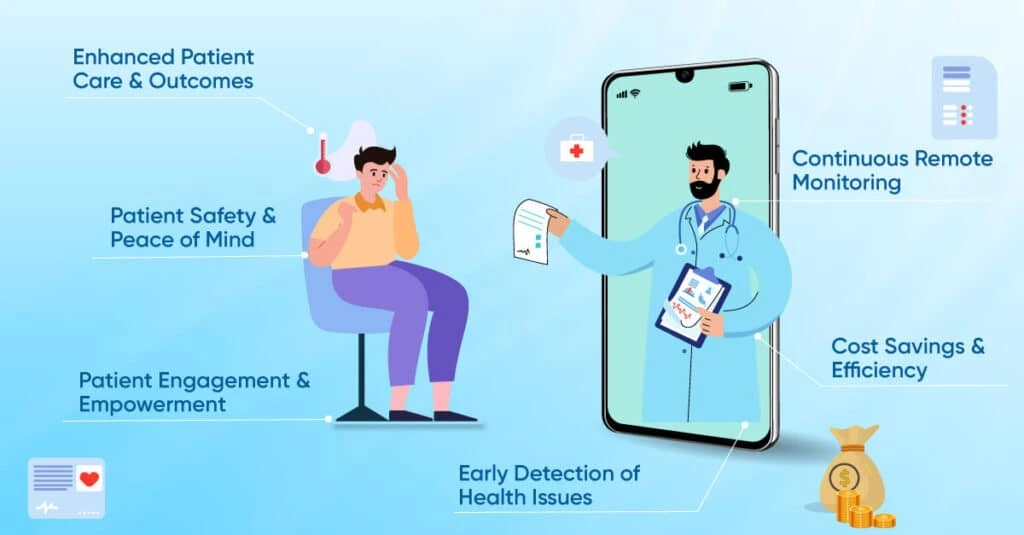
Why RPM Matters
- Early detection of complications: Continuous monitoring allows healthcare providers to catch worsening conditions before they escalate into emergencies.
- Reduced hospital visits: Patients with chronic or complex conditions can avoid unnecessary hospitalizations, reducing costs and inconvenience.
- Improved chronic disease management: Regular data collection helps optimize treatment plans and lifestyle interventions.
- Alleviates healthcare system burden: By shifting monitoring from hospitals to homes, RPM helps healthcare systems focus resources on acute and high-risk cases.
In short, RPM is more than just technology—it represents a shift towards proactive, data-driven, and patient-centric healthcare that is saving lives worldwide.
Why RPM is Becoming Critical — Global & India Context
Global Drivers
1. Rising chronic diseases:
Worldwide, chronic illnesses such as cardiovascular diseases, diabetes, respiratory conditions, and kidney disorders are on the rise due to aging populations, sedentary lifestyles, and longer life expectancy. This surge increases the demand for long-term, continuous care, which traditional healthcare systems often struggle to provide. Remote Patient Monitoring offers a scalable and cost-effective solution, allowing continuous oversight without the constant need for hospital visits. (Grand View Research)
2. Constrained healthcare resources:
Hospitals around the world face challenges such as bed shortages, limited staff, and rising costs. RPM helps alleviate these pressures by enabling home-based monitoring, reducing unnecessary hospital admissions, and allowing healthcare providers to focus on high-risk patients. (Wikipedia)
3. COVID-19 pandemic acceleration:
The pandemic highlighted the need for remote care. Lockdowns, overcrowded hospitals, and infection fears pushed both patients and providers toward telemedicine and RPM solutions. Many healthcare systems now view RPM as a permanent component of care delivery rather than a temporary workaround. (Grand View Research)
India-Specific Context
1. Rapid market growth:
The India RPM market was valued at USD 888.9 million in 2024 and is projected to reach USD 5,428.7 million by 2033, growing at a CAGR of 22.5%. This shows strong adoption potential and increasing investor interest. (Grand View Research)
2. Technology penetration:
With rapid smartphone adoption, increasing internet connectivity, and digital literacy, RPM is becoming feasible even in semi-urban and rural areas. Apps, IoT-enabled devices, and wearable sensors allow real-time monitoring and remote consultations, bridging gaps in India’s healthcare delivery.
3. Addressing India’s chronic disease burden:
India faces a high prevalence of diabetes, hypertension, heart diseases, and respiratory conditions, while healthcare infrastructure struggles to meet demand. RPM offers a viable solution by extending clinical oversight into patients’ homes, reducing hospital congestion, and enabling timely interventions that can prevent complications and save lives.
4. Policy and ecosystem support:
Government initiatives like Ayushman Bharat Digital Mission and increasing investment in digital health startups are creating a supportive environment for RPM adoption, highlighting India’s potential to leapfrog into next-generation healthcare delivery.
In summary:
Globally, RPM is critical to address the rise of chronic diseases, hospital constraints, and post-pandemic care models. In India, rapid technology adoption, high disease burden, and stretched healthcare resources make RPM not just useful, but essential for the future of healthcare delivery.
Clinical Evidence: How RPM is Saving Lives
Remote Patient Monitoring (RPM) is no longer just a promising technology—it is increasingly backed by real-world evidence and peer-reviewed studies demonstrating measurable clinical benefits. Across chronic disease management, post-discharge care, and early detection of complications, RPM has shown the potential to improve outcomes, reduce adverse events, and save lives.
Chronic Disease Management (Diabetes, Hypertension, Heart Disease)
Chronic diseases remain the leading cause of morbidity and mortality worldwide, making effective long-term management essential. RPM helps by providing continuous monitoring, real-time alerts, and digital care coordination.
- A 2025 systematic review focused on chronic diseases in Asia found that internet-based RPM significantly improved patient management, resulting in faster emergency responses, fewer hospitalizations, and optimized clinical outcomes across diabetes, hypertension, and heart disease (Dove Medical Press).
- A 2025 study in a rural California community-health center combined wearable BP monitors, glucometers, and digital care coordination. After six months:
- Hypertensive patients experienced a mean reduction of 20.24 mmHg in systolic blood pressure
- Diabetic patients achieved improved glycemic control (arXiv)
- Hypertensive patients experienced a mean reduction of 20.24 mmHg in systolic blood pressure
These findings highlight that RPM produces clinically meaningful improvements in key metrics. Given that chronic diseases contribute heavily to hospitalizations and mortality globally, RPM can translate into better population-level health outcomes and reduced healthcare costs.
Readmission Reduction & Early Detection
One of RPM’s most life-saving benefits is preventing hospital readmissions and detecting deterioration early:
- UPMC Vivify Health RPM Program:
Medicare patients enrolled in the RPM program were 76% less likely to be readmitted within 90 days post-discharge compared with non-enrolled patients. The program provided home monitoring kits—including BP cuffs, pulse oximeters, and tablets/smartphones—and daily nurse oversight. Alerts triggered timely interventions before emergencies escalated, significantly improving outcomes for elderly and chronic patients (UPMC Enterprises) - A 2024 review of telemonitoring in heart failure (HF) and COPD found that telemonitoring generally reduced readmissions in COPD patients, though HF results were mixed. Even when hospitalizations were not drastically reduced, RPM improved patient satisfaction, continuity of care, and early detection of health deterioration, which together contribute to long-term survival benefits (Frontiers)
Key Insights
- RPM is not merely a convenience tool; it is clinically proven to prevent avoidable hospitalizations.
- It enables early detection of health deterioration, allowing interventions before emergency escalation.
- RPM improves patient satisfaction and continuity of care, which indirectly enhances long-term outcomes and survival rates.
- Particularly for chronic diseases and post-discharge care, RPM represents a scalable, cost-effective method to improve health outcomes while reducing the strain on hospitals.
🔎 Takeaway:
Remote Patient Monitoring transforms healthcare from reactive to proactive care. By continuously tracking vital signs, detecting anomalies early, and coordinating timely interventions, RPM is saving lives, improving chronic disease management, and reducing hospital readmissions globally and in India.
RPM Market Growth & Adoption Trends (Global + India)
| Region / Market Segment | 2024 (or recent) Value | Forecast (2030/2033) & CAGR | Key Insights |
| Global RPM Systems Market | USD 22.03 billion (2024) Grand View Research+1 | USD 110.71 billion by 2033; CAGR ~19.8% Grand View Research+1 | Driven by chronic disease prevalence, rising telehealth adoption, aging population |
| Global RPM Devices Market (2023) | USD 5,178.9 million Grand View Research | USD 16,947.4 million by 2030; CAGR ~18.5% Grand View Research | Vital sign monitors (BP, heart rate, SpO₂) fastest-growing device segment |
| India RPM Market | USD 888.9 million (2024) Grand View Research | USD 5,428.7 million by 2033; CAGR ~22.5% Grand View Research | Fastest-growth market in Asia-Pacific; rising home healthcare demand |
| India RPM Devices (smaller scope) | USD 105.2 million (2023) Grand View Research | USD 452.7 million by 2030; CAGR ~23.2% Grand View Research | Indicates growing consumer uptake of home health devices |
| RPM Software & Services (Global) | USD 8.5 billion (2023) Grand View Research | USD 65.0 billion by 2030; CAGR ~34.9% Grand View Research | Services & software to manage RPM workflows, data analytics, telehealth integration |
Interpretation: The RPM market is growing rapidly across devices, systems, and services — globally and in India. Given India’s high growth rate, increasing digital adoption, and health burden, RPM is poised to become a mainstream mode of care over the next decade.

Key Technologies Enabling RPM
Modern RPM success rests on convergence of several technologies:
- Connected devices and wearables: BP monitors, pulse oximeters, glucometers, heart-rate monitors, multiparameter monitors. These devices capture vital signs and transmit data to platforms — making continuous monitoring possible. Grand View Research+2Wikipedia+2
- Telemedicine & virtual care platforms: RPM platforms integrate data with EHRs, enable alerts, enable video/tele-consultations, and care coordination — essentially enabling “virtual wards.” Wikipedia+2healthrecoverysolutions.com+2
- AI & Predictive Analytics: Academic research shows feasibility of machine-learning models to predict patient deterioration from vital sign data, enabling early intervention before crises. For example, a 2021 study demonstrated a model with AUC-ROC 0.84 for risk-scoring patients based on remote vital data. arXiv+1
- Secure data infrastructure & interoperability: With distributed monitoring comes large data flows — modern RPM systems rely on secure cloud-based infrastructure, sometimes supplemented by blockchain/fog-computing, to ensure patient privacy and timely responses. Grand View Research
- Mobile & internet connectivity: As smartphones and internet connectivity proliferate (especially in emerging markets like India), RPM becomes more accessible — even at home or in rural settings. Grand View Research+1
Challenges & Barriers (Especially for India)
While Remote Patient Monitoring (RPM) has enormous potential to transform healthcare delivery, several challenges and barriers hinder its widespread adoption—particularly in low- and middle-income countries like India. Understanding these obstacles is essential for designing effective RPM strategies and policies.
1. Connectivity & Infrastructure Gaps
- RPM relies on real-time data transmission. In rural and semi-urban areas, internet connectivity can be unreliable, and power supply may be intermittent.
- Without stable broadband or mobile networks, devices like wearable sensors, glucometers, or BP monitors may fail to transmit data consistently, limiting their effectiveness.
- Example: A rural patient with hypertension may not be able to send daily BP readings to their care team due to network outages, leading to missed early warnings.
- Solution: Hybrid models using offline data storage with periodic uploads, low-bandwidth devices, and solar-powered equipment can mitigate some infrastructure gaps.
2. Data Privacy, Security & Regulatory Compliance
- RPM systems collect sensitive health data, including vital signs, medical history, and lifestyle information. This raises critical concerns around privacy, security, and compliance.
- India currently lacks a fully mature health data protection framework, though the proposed Digital Personal Data Protection Act and guidelines from National Digital Health Mission (NDHM) are steps forward.
- Devices and platforms need end-to-end encryption, secure cloud storage, interoperability standards, and compliance with local regulations (Grand View Research).
- Breaches or misuse of health data could erode trust and slow adoption.
3. Adoption & Digital Literacy
- Many RPM users, especially the elderly or less tech-savvy, may struggle with wearable devices, apps, or telehealth platforms.
- Challenges include: difficulty pairing devices, reading digital interfaces, or responding to alerts.
- Successful adoption requires:
- Patient onboarding programs
- Step-by-step training and tutorials
- Ongoing technical support and caregiver involvement
- Patient onboarding programs
4. Healthcare Ecosystem Integration
- Hospitals, clinics, and care teams must adapt workflows to incorporate remote monitoring data into decision-making.
- Without proper integration into Electronic Health Records (EHRs) and clinical care pathways, RPM alerts can overwhelm staff, leading to alert fatigue and underutilization (JAMA Network).
- Effective integration requires:
- Automated alert triaging
- Defined clinical protocols for remote interventions
- Collaboration between primary care, specialists, and RPM monitoring teams
- Automated alert triaging
5. Cost & Affordability
- While RPM devices are becoming more affordable, cost remains a barrier for low-income patients.
- Expenses include hardware, software, connectivity, and subscription fees, which may be prohibitive for large-scale adoption.
- Solutions may involve:
- Government subsidies or insurance coverage
- Low-cost IoT-enabled devices
- Public-private partnerships for community RPM programs
- Government subsidies or insurance coverage
6. Evidence Gap for Certain Conditions
- The clinical effectiveness of RPM is well-established for chronic diseases like diabetes, hypertension, and COPD.
- However, for conditions such as heart failure, mental health, or acute illnesses, evidence is still mixed or limited, and more high-quality, large-scale studies are required (Frontiers).
- Policymakers and hospitals may hesitate to scale RPM programs without robust, condition-specific evidence.
✅ Summary
RPM adoption in India faces a complex mix of technological, regulatory, educational, and economic challenges. Addressing these barriers requires:
- Improving connectivity and device reliability in rural areas
- Strengthening data privacy and regulatory frameworks
- Providing training and ongoing support for patients
- Integrating RPM into clinical workflows effectively
- Ensuring affordability and financial support
- Generating more clinical evidence for a wider range of conditions
With careful planning and policy support, these barriers can be overcome, allowing RPM to reach its full life-saving potential across India.
10-Year Outlook: What’s Next for RPM
Here’s a likely roadmap for RPM adoption and impact through 2035:
🔹 Near-term (2025–2028)
- Continued growth of home-health RPM adoption in urban and semi-urban areas worldwide and in India.
- Rise in hybrid care models — “virtual wards” and “hospital-at-home” — combining teleconsultation, RPM data, and periodic in-person visits. Wikipedia+1
- Wider use of AI and predictive analytics to triage patients and trigger alerts — especially beneficial in overburdened systems. Early AI-RPM studies already show strong potential. arXiv+1
- Integration of RPM data into EHR systems and national/regional health databases (especially in countries investing in digital health).
🔹 Mid-term (2028–2032)
- RPM becomes part of standard chronic disease management protocols for major NCDs (diabetes, hypertension, heart disease).
- Insurance and payers — public and private — begin offering RPM-based care plans or reimbursements, making RPM more affordable and accessible.
- In LMICs (like India), emergence of affordable RPM device-market, possibly aided by local manufacturing, government subsidies or public-private partnerships.
🔹 Long-term (2032–2035)
- RPM widespread even in rural and remote areas; connectivity gaps narrowed thanks to better telecom infrastructure and offline-capable devices.
- Proactive, preventive healthcare becomes common: RPM + AI enables early detection of disease exacerbations, reducing morbidity and mortality.
- Health systems evolve: “hospital-at-home” and virtual wards reduce need for large-scale hospital infrastructure; chronic diseases become more manageable; healthcare costs per capita stabilize or drop.
Best-case scenario: RPM-driven home healthcare becomes mainstream globally, saving millions of lives annually by preventing complications, reducing hospitalizations, and enabling early interventions.
If challenges remain (infrastructure, regulation, cost), adoption may slow — but RPM will still grow steadily, especially in high-income countries and urban areas of emerging economies.
FAQs Section
1. What diseases or conditions benefit most from RPM?
RPM is most effective for chronic and high-risk conditions, including:
- Diabetes – Continuous glucose monitoring allows early detection of hyper- or hypoglycemic events, preventing complications.
- Hypertension – Daily BP tracking helps clinicians adjust medications and detect early signs of cardiovascular risk.
- Heart Disease & Heart Failure – RPM devices like wearables and ECG monitors can detect arrhythmias or fluid retention early.
- Chronic Obstructive Pulmonary Disease (COPD) – Pulse oximeters and respiratory monitors can flag declining lung function.
- Post-surgical or post-discharge patients – Vital sign monitoring prevents readmissions by enabling timely interventions.
Evidence: A 2025 systematic review in Asia confirmed that internet-based RPM improves chronic disease management, reduces hospitalizations, and optimizes clinical outcomes (Dove Medical Press, Wikipedia).
2. Does RPM actually reduce hospital readmissions?
Yes. Multiple studies confirm its effectiveness:
- UPMC Vivify Health Program: Medicare patients enrolled in RPM were 76% less likely to be readmitted within 90 days compared with non-enrolled patients (UPMC Enterprises).
- Systematic Review (2024): Telemonitoring reduced readmissions for COPD patients. Evidence for heart failure is mixed but shows potential benefits for mortality and emergency visit reduction (Frontiers).
3. Can RPM replace in-person doctor visits?
Not entirely. RPM is designed to complement traditional care, not replace it.
- It enables remote monitoring of vitals and early warning detection.
- Reduces the frequency of routine visits, but serious conditions or acute events still require in-person care.
- Example: A patient with heart failure can be monitored daily at home, but may still need hospital intervention during an acute exacerbation.
4. Is RPM safe & secure? What about patient data privacy?
Security is a major concern because RPM collects sensitive health data.
- Modern RPM systems implement encryption, secure cloud storage, and compliance with regulations.
- Advanced technologies like blockchain and fog computing are sometimes used to enhance security (Grand View Research).
- Patients should confirm that data privacy policies are transparent and that providers adhere to local healthcare regulations, especially in India.
5. What technology is needed for RPM at home?
The minimum requirements include:
- Stable internet connection
- Smartphone, tablet, or computer
- Monitoring devices: BP cuff, glucometer, pulse oximeter, heart-rate monitor
For comprehensive RPM, additional tools include: - Multiparameter wearable devices
- AI-enabled analytics platforms
- Integration with Electronic Health Records (EHRs) for clinician oversight (Wikipedia, Health Recovery Solutions).
6. Is RPM affordable — especially in India?
RPM device costs are decreasing, and scaling adoption reduces per-unit cost.
- However, affordability remains a barrier for low-income households.
- Solutions include government subsidies, insurance coverage, or shared cost models.
7. Can RPM work in rural or low-resource settings?
Yes, with caveats:
- Success depends on reliable connectivity, patient training, and support systems.
- Studies show that rural RPM programs with wearables and care coordination significantly improve outcomes (arXiv).
- Hybrid solutions using offline data storage and periodic uploads can overcome network challenges.
8. How reliable is RPM — can it really detect problems early?
RPM is highly reliable when devices are used correctly and monitoring is consistent:
- A 2021 study showed machine-learning models using wearable data achieved AUC-ROC 0.84 in predicting health deterioration (arXiv).
- Early alerts allow clinicians to intervene before emergencies, reducing complications.
- Caveat: Reliability depends on device accuracy, patient adherence, and timely clinician action.
9. What are the main barriers to widespread RPM adoption?
Key challenges include:
- Connectivity and infrastructure gaps
- Data privacy and security concerns
- High device and service costs
- Digital literacy limitations
- Integration into existing healthcare workflows
- Lack of reimbursement or insurance coverage
10. Will RPM replace hospitals in the future?
Unlikely. Hospitals remain essential for acute care, surgeries, and emergencies.
- RPM is transforming chronic disease management, preventive care, and follow-up monitoring.
- The future may see “hospital-at-home” or “virtual ward” models, reducing hospital congestion while improving access (Wikipedia).
11. Is RPM equally effective for all age groups?
RPM benefits older adults and chronic disease patients the most due to frequent monitoring needs.
- Younger or tech-savvy patients can also benefit for preventive care or early detection.
- User-friendly devices and proper onboarding increase adoption across age groups.
12. What should patients consider before enrolling in an RPM program?
Patients should ensure:
- Stable internet connectivity
- Availability of required devices
- Ease-of-use instructions and training
- Clarity on data privacy and how data will be used
- Understanding of when in-person care is required
- Confirmation that data will be actively monitored by qualified clinicians
Summary
- Remote Patient Monitoring (RPM) is more than a convenience — it’s an emerging, evidence-backed lifeline for chronic disease management and post-discharge care.
- The global RPM market is rapidly expanding (USD 22B in 2024 → ~USD 110B by 2033), and the India RPM market is among the fastest growing (CAGR ~22.5%).
- Clinical evidence — from programs like UPMC’s Vivify to recent systematic reviews — demonstrates RPM’s potential to reduce readmissions, improve chronic-disease outcomes, and catch early warning signs.
- Technology enablers (wearables, telehealth, AI, cloud infrastructure) are maturing, making RPM more scalable and cost-effective than ever.
- However, to realize its full potential — especially in India and other LMICs — RPM needs: reliable connectivity, data privacy safeguards, affordable devices, strong clinical integration, and patient education.
- Over the next 5–10 years, RPM could become core to preventive and home-based healthcare — reducing mortality and transforming how we think about chronic illness, hospital care, and access to quality treatment.

Conclusion
Remote Patient Monitoring (RPM) is no longer just a technological innovation—it is a transformative force reshaping modern healthcare. By enabling continuous home-based monitoring, early detection of health deterioration, and proactive chronic-disease management, RPM is not only saving lives but also reducing hospital congestion and healthcare costs.
For countries like India, where chronic diseases such as diabetes, hypertension, and heart disease are highly prevalent and healthcare infrastructure is often stretched, RPM offers a scalable, cost-effective solution that can reach urban and rural populations alike. Real-world studies and peer-reviewed evidence show measurable improvements in blood pressure, glycemic control, readmission reduction, and overall patient outcomes, underscoring its clinical value.
Whether you are a healthcare provider, policymaker, insurer, or patient, the message is clear: the time to adopt RPM is now. Explore pilot programs, integrate RPM into existing care pathways, and leverage technology to create a proactive, patient-centered healthcare system. By embracing RPM today, we can shape the future of healthcare, making it safer, more accessible, and more efficient for everyone.
References
- Grand View Research — Remote Patient Monitoring System Market (Global)
Global RPM systems market valued at USD 22.03 B in 2024, projected to reach USD 110.71 B by 2033 (Read here). - Grand View Research — India RPM Market Outlook
India RPM market valued at USD 888.9 M in 2024, forecasted to reach USD 5,428.7 M by 2033 (Read here). - Grand View Research — RPM Software & Services Market
RPM software & services market estimated at USD 8.5 B in 2023, projected to reach USD 65 B by 2030 (Read here). - PubMed Study — Reducing Hospital Readmissions
Real-world study showing home telemonitoring reduces hospitalizations and ED visits for high-risk post-discharge patients (Read here). - JMIR mHealth and uHealth — RPM Impact on Noncommunicable Diseases
Systematic review demonstrating RPM lowers critical episodes and hospitalizations among chronic disease patients (Read here). - arXiv Preprint — Digital Care Coordination + RPM in Rural Health
RPM with care coordination led to ~20 mmHg systolic BP reduction and better glycemic control over 6 months (Read here). - arXiv — AI for Predicting Patient Interventions
Machine learning model using RPM data achieved AUC‑ROC 0.84 for early detection of deterioration (Read here). - arXiv — IoT-Driven RPM for Cardiac Patients
Low-cost, resource-efficient IoT RPM framework for cardiovascular patients (Read here). - Skyquest Market Insights — RPM Market Forecast
Global RPM market 2024: USD 28.92 B → USD 116.29 B by 2032 (CAGR ~19%) (Read here). - JMIR — Systematic Review on Internet-Based RPM
Confirms RPM improves chronic disease management and reduces hospitalizations in Asia (Read here).