Estimated Reading Time: 40-45 minutes (7,825 words)
Introduction
Digestive issues, anxiety, low immunity, mood swings, fatigue — most people assume these are separate problems. But modern science reveals a powerful truth:
👉 Many of these issues begin in your gut.
Welcome to the gut-brain axis — a two-way communication system where your gut microbiome sends constant signals to your brain, influencing everything from your immunity to your mental health. With over 100 trillion microbes, your gut functions like a “second brain,” producing neurotransmitters, hormones, and immune cells.
In this ultimate 2025 guide, you’ll understand:
✔ How gut-brain communication works
✔ Scientific links to immunity, mood, and cognition
✔ Signs your microbiome is imbalanced
✔ Best foods: prebiotics, probiotics, postbiotics
✔ Indian fermented foods that naturally support gut health
✔ Supplement guide + lifestyle plan
This article is packed with science, real examples, and practical steps — designed for readers worldwide but especially relevant for an Indian audience.
What Is the Gut–Brain Axis?
The gut–brain axis is a complex two-way communication system that links your gastrointestinal (GI) tract with your brain. This network uses nerves, hormones, immune pathways, and gut microbes to send signals back and forth, influencing everything from mood to immunity.
At the center of this connection is the enteric nervous system (ENS) — often referred to as the “second brain.”
- The ENS contains over 500 million neurons, which is more than the spinal cord.
- It operates semi-independently from the central nervous system and controls digestion, motility, enzyme secretion, and gut reflexes.
Why the Gut–Brain Axis Matters
The gut is not just a digestive organ — it actively shapes how you think, feel, and respond to stress. This axis plays a key role in:
- Stress Response
- The gut communicates with the brain through the vagus nerve.
- During stress, gut motility changes, digestion slows, and inflammation may rise.
- The gut communicates with the brain through the vagus nerve.
- Mood Regulation
- The gut microbiome affects neurotransmitters like serotonin, dopamine, and GABA.
- Imbalances can contribute to anxiety, depression, irritability, and mood swings.
- The gut microbiome affects neurotransmitters like serotonin, dopamine, and GABA.
- Immune Function
- Around 70% of the immune system resides in the gut.
- A healthy microbiome trains immune cells, reduces inflammation, and strengthens defenses.
- Around 70% of the immune system resides in the gut.
- Hunger & Satiety
- Gut bacteria influence hormones like ghrelin (hunger) and leptin (fullness).
- They help regulate cravings, metabolism, and appetite.
- Gut bacteria influence hormones like ghrelin (hunger) and leptin (fullness).
- Cognitive Performance
- Microbial metabolites (like SCFAs) support brain function, memory, and focus.
- Gut imbalances are linked with “brain fog” and reduced mental clarity.
- Microbial metabolites (like SCFAs) support brain function, memory, and focus.
A Surprising Fact
More than 90% of your body’s serotonin — the neurotransmitter responsible for happiness, calmness, and emotional well-being — is produced in the gut, not the brain.
This makes gut health essential for stable mood, emotional resilience, and mental wellness.
What Is the Microbiome & Why It Matters?
Your gut microbiome is a vast ecosystem of trillions of microorganisms — including bacteria, fungi, viruses, archaea, and yeasts — that live inside your digestive tract. Collectively, these microbes weigh nearly 1–2 kilograms, making them as significant as an organ.
Each person’s microbiome is unique, shaped by genetics, diet, stress, sleep, medication use, and environmental exposure.
These microorganisms aren’t just passive residents — they actively influence your digestion, metabolism, immunity, mental health, hormone balance, and even your risk of chronic disease. When your microbiome is diverse and balanced, your body thrives. When it becomes disrupted (a state called dysbiosis), multiple systems begin to malfunction.
How a Healthy Microbiome Supports the Body
A strong and diverse gut microbiome plays a critical role in maintaining overall well-being:
✓ 1. Supports Digestion & Nutrient Absorption
- Breaks down complex carbohydrates, fibers, and proteins.
- Produces digestive enzymes and short-chain fatty acids (SCFAs) that nourish the gut lining.
- Helps the body absorb essential nutrients like magnesium, iron, and amino acids.
✓ 2. Strengthens Immunity
- Around 70% of the immune system sits in the gut.
- Beneficial bacteria train immune cells, defend against pathogens, and prevent infections.
- A healthy microbiome keeps inflammation under control.
✓ 3. Produces Essential Vitamins
- Certain gut bacteria create important vitamins, including:
- Vitamin B12 – energy, nerve health
- Vitamin K2 – bone strength, cardiovascular health
- B Vitamins – metabolism, mood regulation
- Vitamin B12 – energy, nerve health
✓ 4. Reduces Inflammation
- Balanced microbes produce anti-inflammatory compounds like butyrate.
- Helps prevent chronic conditions like arthritis, metabolic disorders, and autoimmune issues.
✓ 5. Balances Mood & Brain Chemicals
- Gut bacteria help produce neurotransmitters such as serotonin, dopamine, and GABA.
- They influence mood stability, emotional resilience, and cognitive clarity.
- A healthy microbiome supports lower stress levels and improved mental well-being.
What Happens When the Microbiome Becomes Unhealthy? (Dysbiosis)
When harmful microbes overgrow or beneficial ones decrease, the body experiences a cascade of symptoms.
✗ Digestive Issues
- Bloating, gas, indigestion
- IBS/IBD symptoms
- Constipation or diarrhea
- Food sensitivities
✗ Weak Immunity
- Frequent colds or infections
- Allergies and autoimmune flare-ups
- Slow recovery
✗ Skin Problems
- Acne, dermatitis, eczema
- Rosacea, inflammation
- Poor wound healing
✗ Mood & Mental Health Challenges
- Anxiety, irritability
- Low mood or mood swings
- Increased stress response
- Sleep disturbances
✗ Cognitive Symptoms
- Brain fog
- Poor focus and memory
- Slower processing speed
How the Gut Talks to the Brain (4 Key Pathways)
The communication between your gut and brain isn’t mystical — it happens via several well-studied biological routes. Your gut microbiome, gut nervous system, and immune system all play active roles. Here are the four major pathways through which signals travel from gut → brain (and sometimes brain → gut), along with the “how” and “why it matters.”
🧠 Overview — Why Pathways Matter
- These connections help regulate mood, stress response, digestion, immunity, appetite, cognition, sleep and overall well-being.
- When the gut ecosystem is healthy and balanced, signaling tends to be smooth and beneficial.
- When there’s imbalance or dysbiosis, the same pathways can trigger inflammation, stress-hormone surges, mood swings, “brain fog,” and other issues.
3.1 The Vagus Nerve — The Biological “Superhighway”
What is it?
- The Vagus nerve is a long cranial nerve that connects the gut (and many internal organs) directly to the brain. Roughly 80% of its fibers are afferent (gut → brain), and about 20% are efferent (brain → gut). OUP Academic+2Nature+2
- The gut’s own nervous system — the Enteric nervous system (ENS) — interacts closely with the vagus nerve. The ENS is often called the “second brain.” Psychowellness Center+1
How it works
- Gut microbes influence enteroendocrine and enterochromaffin cells in the gut lining, which release chemical signals (e.g., serotonin, gut hormones like GLP-1, PYY). Nature+2PMC+2
- These signals stimulate vagal afferent fibers, sending information to a brain region called the Nucleus tractus solitarius (NTS) in the brainstem. From there, the signal is processed and relayed to higher-order brain areas that regulate mood, stress, cognition, and autonomic functions. PubMed+2OUP Academic+2
- The vagus nerve also carries signals back to the gut (efferent), regulating gut motility, secretions, and inflammation — thus forming a feedback loop. OUP Academic+1
Why it matters
- Because of this direct, high-speed link, changes in gut microbial activity can affect brain function without needing molecules to cross the blood–brain barrier.
- In animal studies, eliminating the vagus nerve (vagotomy) blocks effects that would otherwise arise from certain probiotic bacteria — confirming that the vagus nerve is critical. OUP Academic+1
- Thus, a balanced, healthy microbiome + gut supports better stress resilience, mood regulation, and overall brain–body harmony.
3.2 Neurotransmitter & Neurochemical Production by Gut Microbes
What’s going on
- Gut microbes (and gut cells influenced by them) can produce or influence the production of key neurotransmitters or neuroactive chemicals — the same chemicals that the brain uses to regulate mood, sleep, appetite, cognition, and more. brainfacts.org+3@WalshMedical+3Cureus+3
- Some of these include:
- Serotonin — often called the “feel-good” neurotransmitter. Around 90% of the body’s total serotonin is synthesized in the gut by gut cells under microbial influence. Cambridge University Press & Assessment+2PMC+2
- Gamma-Aminobutyric Acid (GABA) — an inhibitory neurotransmitter that reduces neural excitability, promoting calm and lowering anxiety. Gut bacteria like certain species of Lactobacillus and Bifidobacterium have been shown to produce GABA. @WalshMedical+2PMC+2
- Dopamine — involved in motivation, reward, and movement. Gut bacteria can influence its synthesis or the availability of its precursors. Nature+2SpringerLink+2
- Acetylcholine, glutamate, and other neurochemicals — studies suggest gut microbes can influence a broader set of neuroactive compounds. Nature+2OUP Academic+2
- Serotonin — often called the “feel-good” neurotransmitter. Around 90% of the body’s total serotonin is synthesized in the gut by gut cells under microbial influence. Cambridge University Press & Assessment+2PMC+2
How those chemicals matter
- Serotonin — regulates mood, sleep, appetite, and gut motility. Disruptions in gut-derived serotonin may influence depression, anxiety, sleep problems, and digestive issues. brainfacts.org+2Cureus+2
- GABA — helps calm the nervous system. Gut-derived GABA is linked to reduced anxiety, better stress handling, and improved relaxation. Lippincott Journals+2SpringerLink+2
- Dopamine & others — may affect motivation, reward-seeking behavior, concentration, and cognitive functions. Gut influence on these pathways might modulate mood disorders and cognitive performance. Nature+2SpringerLink+2
- Even if these gut-derived molecules don’t always cross directly into the brain (because of the blood–brain barrier), they influence the brain indirectly — via the vagus nerve, via immune modulation, via hormone/neuropeptide release, or by affecting the integrity of the gut and blood–brain barrier. Cambridge University Press & Assessment+2PMC+2
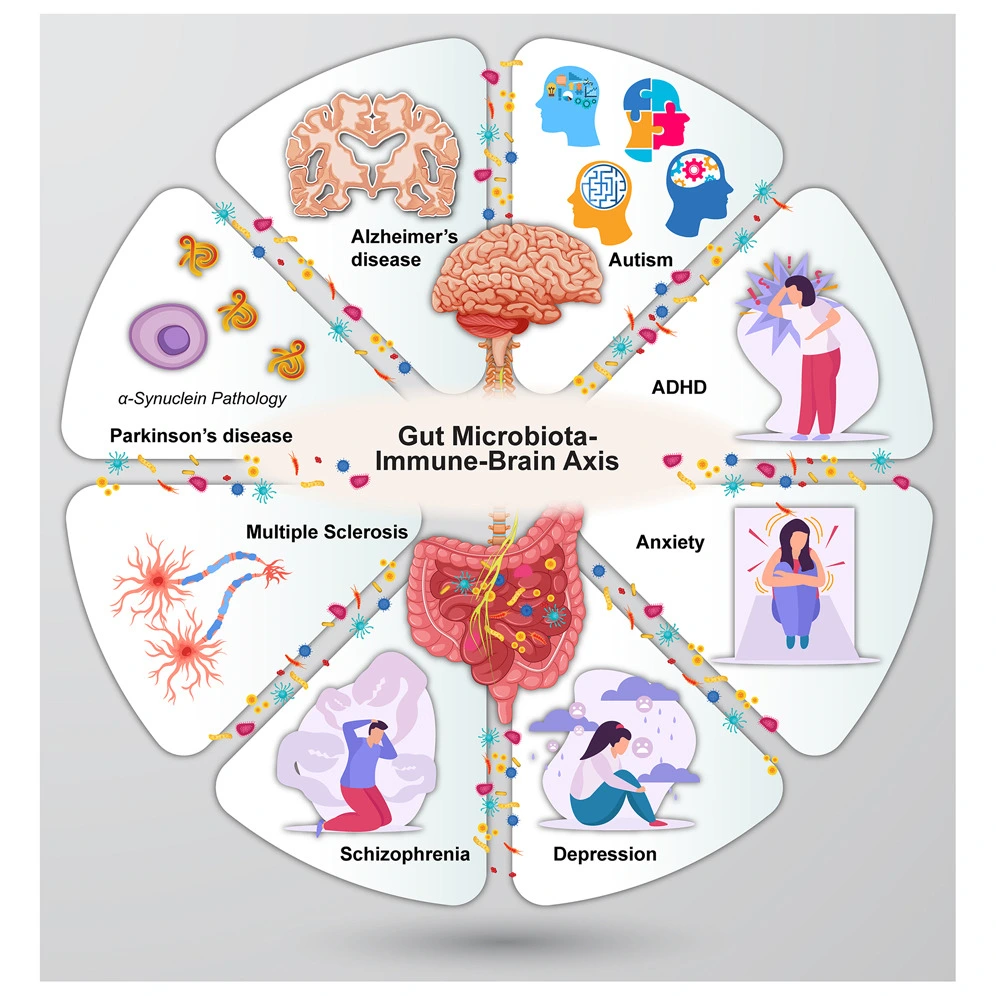
3.3 Immune System & Inflammation — Gut as Immune Headquarters
Gut-immune connections
- A large portion of the body’s immune cells are located in the gut-associated lymphoid tissue (GALT). The gut microbiome plays a central role in shaping immune responses, teaching immune cells which microbes are friendly and which are threats. @WalshMedical+2Nature+2
- Balanced microbes help maintain a healthy gut barrier (intestinal lining), preventing harmful pathogens and toxins from leaking into the bloodstream.
What happens when things go wrong
- When the microbiome is disrupted (dysbiosis) or the gut barrier is compromised (often called “leaky gut”), microbial components or toxins can trigger an immune response. This leads to release of inflammatory molecules (cytokines, immune mediators). PMC+2SpringerLink+2
- These inflammatory signals can circulate systemically and reach the brain, potentially affecting neural function, altering neurotransmitter production, disturbing mood, increasing risk of neuroinflammation, and even contributing to neurodegenerative disease paths. SpringerLink+2OUP Academic+2
Why it matters
- A healthy microbiome can support immune balance, reduce chronic low-grade inflammation, and prevent systemic inflammation that may impair brain health.
- Disturbances in this pathway are increasingly linked to conditions like anxiety, depression, cognitive decline, and neurodegenerative diseases — showing that gut health equals immune health equals brain health. meer.com+2SpringerLink+2
3.4 Microbial Metabolites — The Chemical Messengers (SCFAs, Others)
What are these metabolites?
- When gut microbes digest dietary fiber and complex carbohydrates, they generate short-chain fatty acids (SCFAs) — mainly acetate, propionate, and butyrate. Healthline+2Cambridge University Press & Assessment+2
- They also produce other neuroactive or bioactive metabolites — e.g. from amino-acid fermentation, bile acid transformation, and indole/tryptophan derivatives. SpringerLink+2Mirage News+2
How metabolites influence the brain
- SCFAs and blood–brain barrier (BBB) integrity: Butyrate, in particular, strengthens the blood–brain barrier, protecting the brain from harmful toxins and inflammation. Cambridge University Press & Assessment+1
- Neurotransmitter & neurotrophic modulation: SCFAs can influence gene expression in neurons, support neurogenesis, modulate neurotransmitter systems, and regulate inflammation in the brain. meer.com+2Cambridge University Press & Assessment+2
- Immune and anti-inflammatory effects: SCFAs help regulate immune responses, reduce pro-inflammatory cytokines, and promote production of anti-inflammatory molecules — lowering chronic inflammation that harms both gut and brain. PMC+2Nature+2
Real-world relevance
- Diets low in fiber or high in processed food limit SCFA production, weakening gut-brain communication and increasing risk of gut inflammation, mood disorders, cognitive issues.
- On the other hand, fiber-rich diets, prebiotics (food for beneficial microbes), and probiotic/fermented foods support robust SCFA production — promoting healthier brain and mind.
3.5 Integrated Picture — How the 4 Pathways Work Together
Rather than operating in isolation, all four pathways interplay continuously:
| Trigger / Condition | Gut Activity / Microbiome Response | Combined Output via Gut–Brain Axis | Potential Effect on Brain / Body |
| High-fiber diet + diverse microbiome | SCFA production + microbial metabolism | SCFAs strengthen BBB, support neurotransmitter/gene expression, regulate immune balance; gut microbes modulate ENS & neurochemicals | Better mood, focus, immunity, lower inflammation |
| Balanced probiotics + healthy gut flora | Balanced neurotransmitter precursors, stable ENS signaling, healthy immune modulation | Vagal signaling + neurotransmitter production + immune stability | Stable mood, stress resilience, good digestion |
| Dysbiosis (poor diet, antibiotics, stress) | Reduced beneficial bacteria, gut barrier weakening, inflammatory triggers | Immune activation, altered neurotransmitter balance, disrupted vagal/ENS signaling | Anxiety, depression, brain fog, poor immunity, gut issues |
| Fiber-poor / processed diet with no fermentation | Low SCFAs, limited microbial diversity, poor metabolite production | Weak gut-brain signals, unstable gut hormones/neurochemicals, inflammation | Fatigue, cognitive sluggishness, digestive issues, mood swings |
Because of this synergy, the state of your microbiome becomes central — not just for digestion, but for holistic mind-body balance: immunity, mood, cognition, stress, energy, even hormone regulation.
3.6 What Science Says: Key Evidence & Studies
- Microbiome–gut–brain reviews highlight the vagus nerve as the “central conduit” for gut-to-brain information; in rodents, cutting the vagus nerve abolishes behavioral effects of beneficial bacteria. OUP Academic+2@WalshMedical+2
- Gut microbes influence the enzyme systems in enterochromaffin cells to modulate serotonin synthesis; gut-derived serotonin stimulates vagal afferents, sending signals to brainstem and higher centers. PubMed+2Cambridge University Press & Assessment+2
- Production of SCFAs by gut bacteria can affect blood–brain barrier integrity, neuronal gene expression, and neuroinflammation — thus impacting cognition and mental health. Cambridge University Press & Assessment+2Healthline+2
- Gut dysbiosis is associated with increased inflammatory cytokines, which may reach the brain and contribute to neuropsychiatric and neurodegenerative conditions. PMC+2Nature+2
3.7 What This Means for You — Practical Implications
- A diverse, fiber-rich diet with fermented foods helps nurture beneficial microbes, boosting SCFA production and healthy signaling.
- Avoid long-term misuse of antibiotics, excessive stress, poor diet, and frequent gut irritants — these disrupt microbiome balance and impair gut-brain communication.
- Lifestyle factors — regular sleep, stress reduction, moderate exercise — support healthy ENS and vagal tone, improving gut-brain axis function.
- If considering probiotics or postbiotics, choose well-studied strains (e.g. Lactobacillus, Bifidobacterium) known to produce beneficial neurotransmitters or support gut barrier & immune health.
✅ Summary — Why This Section Matters
Your gut and brain are in constant conversation — not just via thoughts, but via nerves, biochemistry, immune signals, and microbial metabolism. A healthy microbiome means clear lines of communication, stable mood, robust immunity, better digestion, sharper thinking — essentially a foundation for holistic health. Disruption anywhere in this network — gut flora imbalance, low fiber, inflammation — can ripple out and affect your body and mind.
Understanding these pathways is critical if you want to optimize wellness through diet, lifestyle and gut-friendly practices — especially important for readers (like many in India) seeking natural, affordable ways to improve mood, immunity and long-term health.
How Gut Health Impacts Immunity
Your gut microbiome is not just a digestive partner — it is a central regulator of your immune system. Around 70% of immune cells reside in the gut-associated lymphoid tissue (GALT), meaning your gut microbes are in constant dialogue with your immune system. A balanced microbiome can strengthen defenses, reduce chronic inflammation, and even influence how your body reacts to vaccines and pathogens.
1. Fighting Infections Efficiently
- Beneficial gut bacteria act as a first line of defense by:
- Competing with harmful bacteria for space and nutrients.
- Producing antimicrobial compounds like bacteriocins and acids.
- Competing with harmful bacteria for space and nutrients.
- A healthy gut helps immune cells recognize pathogens faster, reducing the severity and duration of infections such as colds, flu, or gastrointestinal illnesses.
- Example: Studies show that individuals with higher gut microbial diversity have lower susceptibility to respiratory infections. (Nature Reviews Immunology, 2023)
2. Vaccine Response & Immunity Boost
- Emerging research suggests that the gut microbiome influences how your body responds to vaccines.
- Beneficial microbes stimulate B-cell and T-cell activity, enhancing antibody production and the effectiveness of vaccines like influenza and COVID-19.
- Real-World Insight: A 2024 Indian study found that children with balanced gut microbiomes produced stronger antibody responses to routine immunizations. (Indian Journal of Pediatrics, 2024)
3. Regulating Inflammation
- Chronic, low-grade inflammation is at the root of many diseases — from heart disease and diabetes to depression and autoimmune disorders.
- A balanced gut microbiome produces short-chain fatty acids (SCFAs) such as butyrate, acetate, and propionate. These molecules:
- Strengthen the gut barrier to prevent “leaky gut.”
- Reduce pro-inflammatory cytokines (e.g., IL-6, TNF-alpha).
- Promote anti-inflammatory immune responses.
- Strengthen the gut barrier to prevent “leaky gut.”
- Key Point: Dysbiosis — an imbalance in gut microbes — increases systemic inflammation, weakening immune defense and promoting disease.
4. Influencing Autoimmune Responses
- The gut microbiome helps train regulatory T-cells (Tregs), which prevent the immune system from attacking healthy tissues.
- Dysbiosis can disrupt this balance, increasing the risk of autoimmune conditions such as:
- Rheumatoid arthritis
- Type 1 diabetes
- Inflammatory bowel disease (IBD)
- Rheumatoid arthritis
- Example: Studies have found that reduced abundance of Faecalibacterium prausnitzii and other anti-inflammatory bacteria correlates with increased autoimmune risk. (Frontiers in Immunology, 2024)
5. How a Balanced Gut Boosts Immunity
A well-maintained gut microbiome supports immunity in multiple ways:
| Benefit | How It Works | Example/Impact |
| Stronger pathogen defense | Competes with harmful microbes, produces antimicrobial compounds | Faster recovery from colds and flu |
| Enhanced vaccine response | Stimulates B & T cells | Higher antibody titers post-vaccination |
| Reduced chronic inflammation | SCFAs regulate cytokine production | Lower risk of metabolic and inflammatory diseases |
| Autoimmune regulation | Tregs trained to prevent self-attack | Lower risk of autoimmune flare-ups |
6. Supporting Gut-Immune Health: Practical Tips
- Eat a fiber-rich diet: Whole grains, legumes, vegetables, and fruits feed beneficial bacteria.
- Include fermented foods: Yogurt, kefir, idli/dosa, kanji, kimchi support probiotics.
- Avoid unnecessary antibiotics: Only use under medical supervision.
- Manage stress: Chronic stress disrupts gut microbes and immune signaling.
- Exercise regularly: Physical activity promotes microbial diversity and immune function.
- Prioritize sleep: 7–8 hours nightly improves gut-immune communication.
Key Takeaways
- Your gut microbiome directly shapes immune strength, inflammation, and vaccine response.
- A balanced gut produces molecules and signals that train immune cells, regulate inflammation, and prevent autoimmunity.
- Diet, lifestyle, and probiotic/prebiotic intake are your most practical tools for maintaining a robust gut-immune axis.
How Gut Health Affects Mood & Mental Health
Your gut doesn’t just digest food — it plays a major role in your mental and emotional well-being. The gut-brain axis allows signals from gut microbes to influence your brain, while stress and emotions can also affect your gut health. When this delicate balance is disrupted, it can contribute to a range of mental health issues.
Impact of Gut Imbalance on Mental Health
An unhealthy gut microbiome, often called dysbiosis, can lead to:
- Anxiety – Imbalanced gut microbes can increase stress hormones like cortisol, making you more prone to nervousness and worry.
- Depression – Reduced diversity of beneficial bacteria may lower serotonin production (over 90% of serotonin is gut-derived), affecting mood and motivation.
- Mood Swings – Fluctuating gut flora can trigger inflammation and neurotransmitter imbalances, leading to irritability or emotional instability.
- Sleep Problems – Gut microbes help regulate melatonin and circadian rhythm; dysbiosis can disrupt sleep patterns.
- Increased Stress Sensitivity – Poor gut health heightens the body’s response to stress, creating a feedback loop that further impacts the gut.

Probiotics & Mood Support
Certain probiotic strains have been studied for their psychobiotic effects — meaning they positively influence mental health:
- Lactobacillus rhamnosus – Shown to reduce anxiety and depressive-like behaviors in animal studies; improves GABA receptor expression in the brain.
- Bifidobacterium longum – Supports stress reduction and emotional regulation; some human trials show lower cortisol levels and improved mood.
- Other beneficial strains – Lactobacillus helveticus, Bifidobacterium bifidum, and multi-strain probiotics have also demonstrated mood-stabilizing effects.
How It Works
- Neurotransmitter Production – Gut bacteria produce serotonin, GABA, dopamine, and other neuroactive compounds.
- Inflammation Modulation – Healthy microbes reduce pro-inflammatory cytokines that can affect the brain.
- Vagus Nerve Signaling – Beneficial bacteria stimulate the vagus nerve to communicate directly with brain regions controlling emotion.
- Stress Hormone Regulation – Gut microbes influence the hypothalamic-pituitary-adrenal (HPA) axis, reducing excessive cortisol release.
Practical Tips for Gut-Mood Health
- Include probiotic foods: Yogurt, kefir, fermented idli/dosa batter, kanji, and kimchi.
- Eat prebiotic-rich foods: Garlic, onions, bananas, and oats feed beneficial microbes.
- Reduce sugar and ultra-processed foods which promote dysbiosis.
- Practice stress management: Meditation, yoga, deep breathing, and regular exercise help maintain a healthy gut-brain axis.
- Consider evidence-based probiotic supplements under guidance if needed.
Key Takeaway
Maintaining a healthy gut microbiome is crucial for emotional stability, reduced anxiety, better stress resilience, and overall mental wellness. By supporting gut balance through diet, lifestyle, and probiotics, you can improve both your mood and cognitive function naturally.
How Gut Bacteria Influence Cognitive Performance
Your gut microbiome doesn’t just affect digestion and mood — it also plays a crucial role in brain function and cognition. Through the gut-brain axis, healthy gut microbes influence focus, memory, learning, and neuroplasticity, while imbalances can contribute to cognitive decline over time.
Ways Healthy Gut Microbes Support Cognitive Performance
- Enhanced Focus and Attention
- Beneficial gut bacteria produce short-chain fatty acids (SCFAs) like butyrate, which reduce inflammation in the brain and improve neural signaling.
- Healthy gut flora helps regulate neurotransmitters such as dopamine and norepinephrine, supporting attention and mental clarity.
- Studies suggest that a diverse microbiome is linked to improved concentration and reduced brain fog. (Frontiers in Neuroscience, 2024)
- Beneficial gut bacteria produce short-chain fatty acids (SCFAs) like butyrate, which reduce inflammation in the brain and improve neural signaling.
- Memory Support
- Gut microbes influence hippocampal function, a brain region critical for memory formation and recall.
- SCFAs and microbial metabolites reduce neuroinflammation, improving short-term and long-term memory.
- Animal studies show that mice with a balanced gut microbiome perform better in memory and maze tests than mice with dysbiosis. (Nature Reviews Neuroscience, 2023)
- Gut microbes influence hippocampal function, a brain region critical for memory formation and recall.
- Learning and Cognitive Flexibility
- A healthy gut promotes neuroplasticity, the brain’s ability to form new neural connections.
- Microbes influence brain-derived neurotrophic factor (BDNF), a protein essential for learning and adaptation.
- Imbalanced gut flora reduces BDNF levels, impairing learning and problem-solving skills.
- A healthy gut promotes neuroplasticity, the brain’s ability to form new neural connections.
- Reducing Chronic Inflammation
- Dysbiosis can trigger low-grade systemic inflammation, which crosses the blood-brain barrier and negatively impacts cognition.
- Chronic inflammation is linked to age-related cognitive decline, Alzheimer’s risk, and slower information processing.
- Maintaining gut health can mitigate these risks by keeping inflammatory markers in check.
- Dysbiosis can trigger low-grade systemic inflammation, which crosses the blood-brain barrier and negatively impacts cognition.
Practical Steps to Support Gut-Driven Cognitive Health
- Eat fiber-rich foods: Vegetables, fruits, whole grains, and legumes feed beneficial microbes.
- Include fermented foods and probiotics: Yogurt, kefir, fermented idli/dosa, kimchi, and sauerkraut.
- Manage stress: Mindfulness, yoga, and regular physical activity promote healthy gut-brain communication.
- Prioritize sleep: 7–8 hours of quality sleep supports microbiome balance and cognitive restoration.
- Limit processed foods and added sugars: These promote dysbiosis and neuroinflammation.
Key Takeaway
Healthy gut bacteria act as cognitive allies — improving focus, memory, learning, and neuroplasticity while reducing inflammation that could impair brain function. By nurturing a diverse and balanced microbiome through diet and lifestyle, you can boost mental performance naturally and reduce the risk of cognitive decline.
Signs of an Unhealthy Gut
Your gut health affects much more than digestion — it influences immunity, mental health, energy levels, skin condition, and even sleep. When the gut microbiome is imbalanced, your body sends multiple warning signals. Recognizing these signs early allows you to take corrective action through diet, lifestyle, and targeted interventions.
1. Persistent Bloating and Gas
- Feeling bloated after almost every meal may indicate an overgrowth of harmful bacteria or difficulty digesting certain foods.
- Excess gas can result from fermentation of undigested food by pathogenic bacteria, especially after high sugar, refined carb, or processed food intake.
- Chronic bloating is also linked to conditions like IBS (Irritable Bowel Syndrome) and small intestinal bacterial overgrowth (SIBO). (Mayo Clinic, 2024)
2. Constipation or Diarrhea
- Frequent constipation may indicate low fiber intake or reduced beneficial bacteria like Bifidobacteria.
- Chronic diarrhea can signal gut inflammation or dysbiosis.
- Alternating constipation and diarrhea is a common symptom of IBS or leaky gut syndrome.
3. Food Intolerances or Sensitivities
- Experiencing bloating, gas, or discomfort after eating certain foods (like dairy, gluten, or high-FODMAP foods) can indicate improper digestion due to microbial imbalance.
- Dysbiosis can increase gut permeability, allowing partially digested food particles to trigger immune reactions.
4. Skin Issues
- Acne, eczema, rosacea, or dry skin can be linked to gut health, sometimes called the gut-skin axis.
- Inflammation and microbial imbalance in the gut may manifest as skin flare-ups, as toxins and inflammatory molecules circulate systemically. (Journal of Dermatological Science, 2024)
5. Fatigue or Low Energy
- Poor gut health can affect nutrient absorption (iron, B12, magnesium), leading to chronic fatigue.
- Dysbiosis may also trigger systemic inflammation, which is associated with persistent tiredness and low motivation.
6. Mood Changes: Anxiety, Irritability, or Depression
- A disturbed gut microbiome can affect neurotransmitter production and the gut-brain axis, leading to:
- Increased stress sensitivity
- Mood swings or irritability
- Anxiety or depressive symptoms
- Increased stress sensitivity
- Certain probiotic strains, like Lactobacillus rhamnosus and Bifidobacterium longum, are known to reduce anxiety and improve emotional well-being.
7. Poor Sleep or Insomnia
- Gut microbes influence melatonin production, the hormone that regulates sleep-wake cycles.
- Dysbiosis can disrupt circadian rhythms, making it harder to fall asleep or stay asleep.
8. Frequent Infections
- Since 70% of your immune system resides in the gut, microbial imbalance can impair immune responses.
- People with unhealthy gut microbiomes are more prone to colds, flu, urinary tract infections, and other infections.
9. Additional Subtle Signs
- Cravings for sugar or processed foods — often due to gut microbes “training” your brain for their preferred nutrients.
- Bad breath or dental issues — linked to oral and gut microbial imbalance.
- Weight fluctuations — gut dysbiosis can affect metabolism and fat storage.
Key Takeaway
Your gut sends signals long before serious illness develops. Persistent digestive discomfort, fatigue, skin problems, mood disturbances, sleep issues, or frequent infections are all red flags of a microbiome imbalance. Early recognition, combined with dietary changes, probiotics/prebiotics, stress management, and lifestyle adjustments, can restore gut balance and improve overall health.
Prebiotics, Probiotics, Postbiotics — Explained
Maintaining a healthy gut microbiome relies on a combination of prebiotics, probiotics, and postbiotics. Each plays a distinct role in supporting digestion, immunity, mood, and overall health. Understanding the differences helps you make informed dietary choices.
1. Prebiotics — Food for Your Gut Bacteria
- What they are: Prebiotics are non-digestible fibers that serve as fuel for beneficial gut microbes. They pass through the small intestine undigested and are fermented by bacteria in the colon, producing short-chain fatty acids (SCFAs) that support gut and brain health.
- Health benefits:
- Promote growth of beneficial bacteria like Bifidobacteria and Lactobacillus.
- Reduce inflammation and improve immune function.
- Support mineral absorption (calcium, magnesium).
- Help regulate appetite and blood sugar.
- Promote growth of beneficial bacteria like Bifidobacteria and Lactobacillus.
- Food sources: Onions, garlic, leeks, asparagus, oats, bananas, apples, and whole grains.
- Tip: Incorporate prebiotics gradually to avoid excessive gas or bloating.
2. Probiotics — Live Beneficial Bacteria
- What they are: Probiotics are live microorganisms that confer health benefits when consumed in adequate amounts. They help balance the gut microbiome by adding more beneficial bacteria.
- Health benefits:
- Aid digestion and reduce IBS symptoms.
- Enhance immunity and reduce risk of infections.
- Support mood regulation via the gut-brain axis.
- Reduce chronic inflammation and strengthen the gut barrier.
- Aid digestion and reduce IBS symptoms.
- Food sources:
- Dairy-based: Yogurt, kefir, buttermilk.
- Fermented foods: Kimchi, sauerkraut, dosa/idli batter, kanji.
- Beverages: Kombucha, fermented teas.
- Dairy-based: Yogurt, kefir, buttermilk.
- Tip: Look for products labeled with live and active cultures. Strain-specific benefits (e.g., Lactobacillus rhamnosus for mood, Bifidobacterium longum for stress) can be considered.
3. Postbiotics — The Powerful Metabolic By-Products
- What they are: Postbiotics are bioactive compounds produced when probiotics digest fibers or ferment food. These include SCFAs (butyrate, acetate, propionate), enzymes, peptides, and other metabolites.
- Health benefits:
- Strengthen the gut barrier and prevent “leaky gut.”
- Reduce inflammation and oxidative stress.
- Support immune function and overall metabolic health.
- Influence mood, cognition, and neuroprotection via gut-brain communication.
- Strengthen the gut barrier and prevent “leaky gut.”
- Sources:
- Naturally present in fermented foods.
- Some supplements provide concentrated postbiotic compounds.
- Naturally present in fermented foods.
- Tip: Even if probiotics don’t survive digestion fully, their postbiotic effects can still benefit gut and overall health.
How They Work Together
| Component | Role in Gut Health | Examples |
| Prebiotics | Feed beneficial bacteria and support SCFA production | Garlic, oats, bananas, apples |
| Probiotics | Introduce live beneficial bacteria | Yogurt, kefir, kimchi, idli batter |
| Postbiotics | Provide bioactive compounds for immunity, mood, and gut barrier | SCFAs from fermented foods, certain supplements |
Key Point: Combining prebiotics, probiotics, and postbiotics — often called the 3-P approach — ensures a balanced and resilient microbiome, improving digestion, immunity, mood, and cognitive performance.
Best Foods for Gut Health (India-Friendly List)
A diverse, fiber-rich, and fermented diet is key to supporting a healthy gut microbiome. Including a mix of prebiotic, probiotic, and postbiotic-rich foods can help digestion, immunity, mood, and cognitive function. Here’s an India-focused guide to the best options:
A. Prebiotic Foods — Feed Your Good Bacteria
Prebiotics are non-digestible fibers that act as food for beneficial gut microbes. They enhance microbial diversity and promote the production of short-chain fatty acids (SCFAs) that support gut and brain health.
Top India-Friendly Prebiotic Foods:
- Garlic – Stimulates growth of beneficial bacteria like Bifidobacteria; supports immunity and inflammation control.
- Onions & Leeks – Rich in inulin, a prebiotic fiber that fuels gut microbes.
- Green Banana Flour / Raw Bananas – High in resistant starch, improving gut motility and SCFA production.
- Whole Grains – Brown rice, millets (ragi, jowar, bajra) feed healthy microbes and improve digestion.
- Oats – Beta-glucan fibers enhance microbial diversity and reduce cholesterol.
- Apples – Contain pectin, a soluble fiber that boosts Lactobacilli growth.
Tip: Combine multiple prebiotic foods daily for maximum microbial diversity.
B. Probiotic Foods — Add Beneficial Bacteria
Probiotics are live microorganisms that balance your gut flora, improve digestion, and influence mood via the gut-brain axis.
Top India-Friendly Probiotic Options:
- Curd (Dahi) – Traditional Indian yogurt; rich in Lactobacillus species. Best homemade to avoid excess sugar and preservatives.
- Lassi / Buttermilk – Fermented dairy drinks with active cultures that support immunity and hydration.
- Kanji – Fermented carrot or beetroot drink, naturally probiotic-rich.
- Homemade Pickles (Achar) – Traditionally fermented without excessive vinegar or preservatives; contains lactic acid bacteria.
- Idli/Dosa Batter – Naturally fermented rice and lentil batter; rich in beneficial microbes.
- Kombucha – Fermented tea containing probiotics and organic acids.
- Yakult-Type Drinks – Commercial probiotic beverages; check sugar content before regular consumption.
Tip: Include at least one probiotic source daily, preferably fermented at home or minimally processed.
C. Postbiotic-Rich Foods — Microbial Metabolic By-Products
Postbiotics are bioactive compounds produced by probiotic bacteria. They support gut barrier integrity, reduce inflammation, and improve immunity and brain health.
Top Postbiotic Foods:
- Miso – Fermented soybean paste used in soups; rich in SCFAs and peptides.
- Kimchi – Spicy fermented cabbage; contains SCFAs and bioactive compounds.
- Tempeh – Fermented soy product high in protein and postbiotic metabolites.
- Fermented Soy Products – Traditional soy-based ferments in Indian and East Asian diets support gut barrier and immunity.
Tip: Even if probiotics do not survive digestion, postbiotics produced during fermentation still provide gut and systemic benefits.
D. Quick Daily Indian Gut-Friendly Meal Ideas
- Breakfast: Idli or dosa with coconut chutney + green banana smoothie.
- Mid-morning snack: Apple or oat-porridge with chia seeds.
- Lunch: Millet-based roti with garlic/onion sabzi + homemade curd.
- Evening drink: Kanji or lassi.
- Dinner: Brown rice with fermented soybean curry (tempeh or miso) + lightly sautéed vegetables.
- Optional: Small serving of kimchi or homemade pickle to enhance microbial diversity.
Key Takeaways
- Include a variety of prebiotic, probiotic, and postbiotic foods daily.
- Homemade and minimally processed options are preferred to maximize live microbial content.
- A diet rich in fibers, fermented foods, and traditional Indian staples helps maintain a resilient gut microbiome, supporting digestion, immunity, mood, and cognitive function.
Indian Fermented Foods (Easy Recipes)
Fermented foods are a cornerstone of traditional Indian diets and a natural way to boost gut health. They provide live probiotics, postbiotics, and SCFAs, which support digestion, immunity, mood, and cognitive function. Here are some easy Indian fermented foods you can prepare at home with minimal effort:
1. Beetroot Kanji
What it is: A traditional North Indian fermented drink made from beetroot, black mustard seeds, and water.
Benefits:
- Rich in lactic acid bacteria, which act as probiotics.
- Provides antioxidants, supports liver detox, and promotes gut microbial diversity.
- Boosts digestion and immunity.
Easy Recipe:
- Wash and peel 3–4 medium beetroots. Cut into thin strips.
- Dissolve 1–2 tsp black mustard seeds in 500 ml water. Add a pinch of salt.
- Place beetroot strips in a sterilized glass jar and pour the mustard-water solution over them.
- Cover with a cloth and ferment at room temperature for 3–5 days.
- Once sour and slightly fizzy, store in the refrigerator.
- Dosage: Drink 100–150 ml per day before meals.
Tip: You can experiment by adding grated carrots or ginger for extra flavor and microbial variety.
2. Homemade Curd (Dahi)
What it is: Naturally fermented milk containing live Lactobacillus cultures.
Benefits:
- Improves digestion, especially lactose breakdown.
- Enhances immunity and balances gut bacteria.
- Supports calcium absorption for bone health.
Easy Recipe:
- Boil 1 liter of milk and let it cool to 40–45°C.
- Add 2–3 tbsp of existing curd as a starter. Mix gently.
- Cover and keep in a warm place for 6–8 hours or overnight until it sets.
- Dosage: 100–200 ml daily, plain or with fruits.
Tip: For a thicker probiotic-rich curd, use full-fat milk and avoid stirring until fully set.
3. Idli/Dosa Batter
What it is: Fermented rice and urad dal (split black gram) batter used for South Indian staples.
Benefits:
- Naturally rich in Lactobacillus and Bifidobacterium species.
- Improves nutrient bioavailability (iron, B vitamins).
- Supports gut microbiome diversity and postbiotic production.
Easy Recipe:
- Soak 2 cups rice and 1 cup urad dal separately for 4–6 hours.
- Grind into smooth pastes, then mix together.
- Add a pinch of salt and let the batter ferment overnight or 8–12 hours in a warm spot.
- Use the batter for idli or dosa.
Tip: For enhanced probiotic benefits, ferment longer in cooler climates or use a warm yogurt starter.
4. Amla Pickle (Natural Fermentation)
What it is: A traditionally fermented Indian pickle using Indian gooseberry (amla).
Benefits:
- Rich in Vitamin C, antioxidants, and probiotics.
- Supports immunity, digestion, and gut microbial diversity.
- Acts as a natural anti-inflammatory agent.
Easy Recipe:
- Wash and chop 500g fresh amla. Remove seeds.
- Mix with 2 tsp salt and 1 tsp turmeric powder. Optional: add mustard seeds or chili powder.
- Place in a sterilized glass jar and cover loosely.
- Ferment at room temperature for 7–10 days, shaking gently every day.
- Once sour and slightly effervescent, store in the refrigerator.
Tip: Combine with other vegetables like carrots or radish for a mixed fermented pickle rich in probiotics.
5. Additional Indian Fermented Options
- Kanji with Carrot & Radish – adds more microbial diversity.
- Fermented Soy (Tempeh) – easy to incorporate in curries.
- Dhokla Batter – fermented gram flour, probiotic-friendly.
Key Takeaways
- Fermentation is a natural probiotic booster — it enhances gut microbial diversity, supports immunity, reduces inflammation, and improves digestion.
- Traditional Indian foods like kanji, curd, idli/dosa, and amla pickle are easy to prepare at home and affordable.
- Including 1–2 fermented foods daily can help maintain a balanced gut microbiome, improve mood, and even support cognitive function.
Supplement Guide (Safe Recommendations)
While a balanced diet with prebiotic, probiotic, and postbiotic foods is the foundation of gut health, supplements can help bridge gaps, especially for busy lifestyles, stress, or digestive issues. Here’s a practical guide to safe, effective gut health supplements.
A. Probiotics — Live Beneficial Bacteria
Purpose: Probiotics introduce live microorganisms into your gut to improve microbial diversity, support digestion, immunity, and mood, and reduce inflammation.
Key Guidelines for Choosing Probiotics:
- CFU Count: Look for supplements with 5–10 billion CFU (colony-forming units) per serving for general gut health. Higher CFU counts may be recommended for specific conditions under medical supervision.
- Multi-Strain Blends: Choose formulations that include both Lactobacillus and Bifidobacterium species, as different strains support digestion, immunity, and mood in complementary ways.
- Delayed-Release Capsules: Protect the bacteria from stomach acid so more survive to colonize the intestines.
- Indian Market Options:
- Yakult probiotic drinks (single strain, widely available)
- Culturelle, Garden of Life, or Florisia multi-strain capsules (available online)
- Yakult probiotic drinks (single strain, widely available)
- Dosage: Usually 1 capsule/day or as directed; follow label instructions for strain-specific benefits.
Tip: Store probiotics in a cool, dry place, or in the fridge if recommended, to maintain potency.
B. Prebiotic Supplements — Feed Your Good Bacteria
Purpose: Prebiotics are non-digestible fibers that selectively feed beneficial gut bacteria and boost SCFA production.
Common Prebiotic Supplements:
- Inulin: Derived from chicory root or Jerusalem artichoke; supports Bifidobacteria.
- FOS (Fructo-Oligosaccharides): Short-chain prebiotic fiber; improves gut microbial diversity.
- Acacia Gum (Gum Arabic): Gentle on the stomach; helps with constipation and microbial balance.
Dosage & Tips:
- Start with small amounts (1–2 grams/day) and gradually increase to avoid bloating or gas.
- Combine prebiotics with a probiotic for synbiotic effect — feeding the microbes you introduce.
Indian Context: Some local powders and ayurvedic preparations (like psyllium husk/fiber supplements) can act as natural prebiotics.
C. Postbiotic Supplements — Bioactive Compounds for Gut & Immune Health
Purpose: Postbiotics are metabolic by-products of probiotics (e.g., SCFAs, peptides) that support the gut barrier, immunity, inflammation control, and brain function.
Common Postbiotic Supplements:
- Butyrate Supplements: SCFA that supports gut lining and reduces inflammation.
- Heat-Killed Bacterial Extracts: Non-viable probiotics that still trigger immune benefits safely.
- Polyphenol-Based Postbiotics: Some plant-derived supplements (green tea extract, polyphenol-rich berry powders) support gut microbial metabolism.
Tip: Postbiotics are generally stable and safe, even when stomach acid would normally destroy live probiotics.
D. Safety Precautions
- Always consult a doctor if you are:
- Pregnant or breastfeeding
- Immunocompromised
- On antibiotics or other medications
- Pregnant or breastfeeding
- Supplements should complement a healthy diet, not replace it.
- Track your response: Some people may experience mild bloating, gas, or stool changes initially.
E. Practical Supplement Routine (Example)
| Time | Supplement | Notes |
| Morning | Probiotic capsule | On an empty stomach or as per label |
| With Breakfast | Prebiotic powder (Inulin/FOS) | Mix in oats, smoothies, or milk |
| Optional | Postbiotic supplement | Especially for stress, immune support, or chronic inflammation |
Key Takeaway: Combining prebiotics, probiotics, and postbiotics thoughtfully can strengthen your gut microbiome, support immunity, improve digestion, and enhance mental well-being. Always prioritize quality, strain-specific benefits, and safety.
Lifestyle Habits to Strengthen the Gut
Maintaining a healthy gut microbiome is not just about diet and supplements — daily lifestyle habits play a critical role in digestion, immunity, mood, and cognitive health. Small, consistent changes can help your gut thrive, leading to long-term benefits.
1. Prioritize Sleep: 7–8 Hours Daily
- Why it matters: Gut microbes have their own circadian rhythm, which interacts with your body’s internal clock. Poor sleep can disrupt microbial balance, increase inflammation, and impair metabolism.
- Tips for Better Sleep:
- Maintain a consistent bedtime and wake-up time.
- Limit late-night heavy meals, sugar, and caffeine.
- Practice relaxation techniques like meditation, deep breathing, or light yoga before bed.
- Maintain a consistent bedtime and wake-up time.
- Impact: Adequate sleep improves digestion, immunity, and mental clarity.
2. Reduce Sugar and Ultra-Processed Foods
- Why it matters: Excess sugar feeds pathogenic gut bacteria and yeast, leading to dysbiosis. Processed foods with preservatives and emulsifiers also harm microbial diversity.
- Tips:
- Minimize sugary drinks, packaged snacks, and ready-to-eat meals.
- Replace with whole fruits, nuts, seeds, and traditional Indian snacks like roasted chana or makhana.
- Minimize sugary drinks, packaged snacks, and ready-to-eat meals.
- Impact: Reducing sugar stabilizes blood sugar, improves gut flora, and reduces inflammation.
3. Follow a High-Fiber Diet
- Why it matters: Dietary fiber acts as a prebiotic, feeding beneficial bacteria and promoting SCFA production, which supports gut lining, immunity, and brain function.
- India-Friendly Sources:
- Whole grains: Ragi, jowar, bajra, brown rice, oats
- Pulses & lentils: Moong dal, masoor dal, chana dal
- Vegetables & fruits: Leafy greens, carrots, apples, bananas, guava
- Whole grains: Ragi, jowar, bajra, brown rice, oats
- Tip: Include both soluble and insoluble fibers for optimal gut motility and microbial diversity.
4. Stay Hydrated
- Why it matters: Water supports digestion, nutrient absorption, and stool consistency, preventing constipation.
- Tips:
- Aim for 2–3 liters/day, including herbal teas and water-rich fruits/vegetables.
- Avoid excessive caffeine or sugary drinks, which can dehydrate.
- Aim for 2–3 liters/day, including herbal teas and water-rich fruits/vegetables.
- Impact: Proper hydration helps the gut microbiome thrive and supports toxin elimination.
5. Exercise Regularly: 20–30 Minutes Daily
- Why it matters: Physical activity increases gut microbial diversity, improves motility, reduces inflammation, and lowers stress hormones.
- Tips:
- Activities: Brisk walking, yoga, cycling, strength training, or traditional Indian forms like Surya Namaskar.
- Consistency matters more than intensity — aim for moderate activity most days of the week.
- Activities: Brisk walking, yoga, cycling, strength training, or traditional Indian forms like Surya Namaskar.
- Impact: Regular exercise supports digestion, immunity, mood, and metabolic health.
6. Reduce Unnecessary Antibiotics and Painkillers
- Why it matters: Antibiotics kill both harmful and beneficial bacteria, leading to dysbiosis. Long-term use of NSAIDs (painkillers) can irritate the gut lining.
- Tips:
- Only take antibiotics under medical supervision.
- Use painkillers sparingly, and consider natural anti-inflammatory options (turmeric, ginger).
- Only take antibiotics under medical supervision.
- Impact: Minimizing these drugs helps maintain a resilient gut microbiome and prevents digestive issues.
7. Manage Stress Effectively
- Why it matters: Chronic stress disrupts the gut-brain axis, altering microbial composition and increasing inflammation.
- Stress Management Techniques:
- Mindfulness meditation or guided breathing exercises
- Yoga, pranayama, or Surya Namaskar
- Regular outdoor walks in natural settings
- Journaling or gratitude practices
- Mindfulness meditation or guided breathing exercises
- Impact: Lower stress supports healthy digestion, mood, and immune function.
8. Additional Lifestyle Tips for Gut Health
- Chew food thoroughly to aid digestion and nutrient absorption.
- Eat meals at regular times to maintain circadian rhythm for gut microbes.
- Include fermented foods daily for a steady supply of probiotics and postbiotics.
- Limit late-night heavy meals and alcohol, which disrupt gut flora.
Key Takeaways
- Gut health is holistic — diet, sleep, exercise, hydration, stress management, and mindful medication use all contribute.
- Small, consistent lifestyle changes — like 7–8 hours of sleep, high-fiber meals, daily probiotics, hydration, and moderate exercise — can dramatically improve your digestion, immunity, mood, and cognitive function.
- Combine these habits with fermented foods and supplements for a fully balanced gut microbiome.
FAQs Section
1. Does gut health really affect mental health?
Absolutely. The gut produces neurotransmitters such as:
- Serotonin (~90% produced in the gut) – regulates mood and sleep.
- GABA – promotes calmness and reduces anxiety.
- Dopamine – supports motivation and reward pathways.
An imbalanced gut (dysbiosis) increases systemic inflammation and stress hormones like cortisol, contributing to anxiety, depression, mood swings, and brain fog.
Evidence: Studies show that Lactobacillus rhamnosus and Bifidobacterium longum supplementation can reduce anxiety and depressive symptoms in both humans and animal models. (Frontiers in Psychiatry, 2023)
Actionable Tip: Include a variety of prebiotic and probiotic foods daily, manage stress, and consider evidence-backed probiotic supplements.
2. Can probiotics treat anxiety or depression?
Probiotics are not a replacement for therapy or medication, but certain strains — called psychobiotics — can help:
- Reduce stress-induced inflammation
- Modulate the HPA axis (stress hormone regulation)
- Support neurotransmitter balance
Example: Lactobacillus helveticus + Bifidobacterium longum reduced anxiety scores in several clinical trials over 4–8 weeks.
Tip: Pair probiotic intake with healthy diet, sleep, and exercise for best mental health outcomes.
3. How long does it take to improve gut health?
Improvements are gradual and depend on consistency:
- 2–6 weeks: Noticeable changes in digestion, energy, and mood.
- 6–12 weeks: Microbiome diversity improves; immunity and inflammation markers normalize.
- 6+ months: Long-term habits stabilize microbial balance and cognitive benefits.
Tip: Track bowel patterns, energy levels, and mood to monitor progress.
4. Can children take probiotics?
Yes — but:
- Use age-appropriate strains and doses.
- Consult a pediatrician, especially for infants, toddlers, or immunocompromised children.
Example: Lactobacillus rhamnosus GG is widely studied in children for digestive health and immunity.
Tip: Include naturally fermented foods like curd, idli/dosa, and kanji in a child’s diet for gentle probiotic support.
5. Is curd enough as a probiotic?
Curd (dahi) is a good source of Lactobacillus, but:
- It may not provide a diverse strain profile needed for full gut health benefits.
- Commercial curds often have lower live bacterial counts or added preservatives.
Tip: Combine curd with other fermented foods (kanji, dosa/idli batter, pickles) and/or supplements for broader microbial support.
6. Do antibiotics damage gut bacteria?
Yes — antibiotics are non-selective, killing both harmful and beneficial bacteria.
- Can lead to dysbiosis, bloating, diarrhea, and lowered immunity.
- Recovery typically takes 4–6 weeks, aided by probiotics and a high-fiber diet.
Tip:
- Take probiotics a few hours after antibiotics.
- Include prebiotic foods to help beneficial bacteria recolonize.
7. What causes sudden gut imbalance?
Common triggers include:
- Dietary factors: High sugar, ultra-processed foods, low fiber
- Stress & poor sleep
- Medications: Antibiotics, painkillers (NSAIDs)
- Alcohol overuse
- Infections or illness
Tip: Identify triggers and restore balance using fermented foods, prebiotic fiber, hydration, and stress management techniques.
8. Are probiotic supplements safe long-term?
Generally, yes — especially multi-strain probiotics with 5–10 billion CFU.
- Rotation: Some experts suggest rotating strains every few months for diverse microbial support.
- Safety: Avoid in immunocompromised individuals without medical supervision.
Tip: Always follow label instructions and pair supplements with a balanced, fiber-rich diet.
9. What is a gut detox?
Real gut detox is not juice cleanses — it’s about:
- Removing gut irritants: excess sugar, ultra-processed foods, alcohol
- Supporting digestion with fiber-rich foods and fermented foods
- Staying hydrated and exercising
- Restoring microbial balance via probiotics and prebiotics
Tip: Consistent dietary and lifestyle changes are far more effective than short-term cleanses.
10. Is kombucha safe for everyone?
Kombucha is safe for most healthy adults, providing probiotics and postbiotic compounds.
- Caution: Avoid if pregnant, breastfeeding, immunocompromised, or prone to GI upset.
- Tip: Start with 50–100 ml/day, homemade or low-sugar store-bought versions.
11. Can gut health affect immunity?
Absolutely. About 70% of immune cells reside in the gut:
- Balanced gut flora supports vaccine response, pathogen defense, and reduces inflammation.
- Dysbiosis increases susceptibility to infections and autoimmune flare-ups.
Tip: Combine prebiotic fiber, probiotics, fermented foods, and postbiotics for immune resilience.
12. Are there Indian foods that act as natural probiotics?
Yes — traditional Indian foods are rich in live cultures:
- Curd, lassi, buttermilk
- Idli/dosa batter
- Kanji (fermented carrot/beetroot drink)
- Homemade pickles
- Dhokla & fermented soy products (tempeh, miso)
Tip: Include 1–2 servings daily for consistent probiotic intake.
Key Takeaways from FAQs
- Gut health affects digestion, immunity, mood, and cognition.
- Diet, lifestyle, and targeted supplements can restore microbial balance.
- Traditional Indian foods and fermented preparations are affordable, effective, and safe for most adults and children.
- Consistency over weeks to months is key for long-term gut-brain benefits.
Summary
- The gut-brain axis is a bidirectional communication system linking the digestive tract and the brain, influencing mood, stress response, immunity, and cognition.
- The microbiome — trillions of bacteria, fungi, and microorganisms in the gut — plays a crucial role in digestion, vitamin production, immune function, and inflammation control.
- Gut imbalance (dysbiosis) can lead to bloating, constipation, diarrhea, food intolerances, skin issues, fatigue, brain fog, and mood disorders like anxiety or depression.
- Gut microbes influence the brain through four key pathways: the vagus nerve, neurotransmitter production, immune system interactions, and microbial metabolites such as short-chain fatty acids (SCFAs).
- Maintaining gut health strengthens immunity, improving infection resistance, vaccine response, and lowering chronic inflammation.
- A healthy gut positively impacts mental health and cognitive performance, supporting memory, focus, learning, and neuroplasticity.
- Prebiotics, probiotics, and postbiotics are essential for microbial balance:
- Prebiotics: Fiber-rich foods like garlic, onions, oats, and bananas feed beneficial bacteria.
- Probiotics: Live bacteria from curd, lassi, kanji, idli/dosa, and fermented foods help restore gut flora.
- Postbiotics: Metabolic by-products from fermented foods improve immunity and gut barrier function.
- Prebiotics: Fiber-rich foods like garlic, onions, oats, and bananas feed beneficial bacteria.
- India-friendly fermented foods like beetroot kanji, homemade curd, idli/dosa batter, and amla pickle provide easy, natural probiotic support.
- Supplements can complement diet, with careful attention to probiotic strains, CFU count, prebiotic fibers, and postbiotic formulations. Consult a doctor if pregnant, immunocompromised, or on medication.
- Lifestyle habits — sufficient sleep, hydration, regular exercise, stress management, fiber-rich diet, and minimizing sugar, alcohol, and unnecessary antibiotics — are critical for gut resilience.
- Overall, nurturing the gut microbiome through diet, lifestyle, and fermented foods supports immunity, mental health, cognitive function, and long-term well-being.
Conclusion
The gut-brain axis is a powerful network connecting our digestive system and brain, influencing not only digestion but also immunity, mood, and cognitive function. A balanced gut microbiome — supported by prebiotics, probiotics, postbiotics, and fermented foods — plays a crucial role in maintaining overall health. Dysbiosis or an unhealthy gut can manifest as digestive discomfort, fatigue, mood swings, poor sleep, and even cognitive decline, highlighting the importance of proactive gut care.
Integrating traditional Indian fermented foods, fiber-rich diets, and targeted supplements can help restore microbial balance, while lifestyle factors such as stress management, adequate sleep, regular exercise, and hydration further strengthen gut health. The combination of diet, probiotics, and mindful living not only improves digestive wellness but also supports mental clarity, emotional stability, and robust immunity.
Ultimately, gut health is central to holistic well-being. By understanding the gut-brain connection and adopting simple, consistent practices — from including curd, kanji, and idli/dosa in meals to reducing sugar and processed foods — readers can actively nurture their gut microbiome. These small, sustainable steps can lead to lasting improvements in digestion, mood, cognition, and overall quality of life, making gut health a cornerstone of everyday wellness.
References
- Harvard Health Publishing – The gut-brain connection: How it works and why it matters.
https://www.health.harvard.edu/diseases-and-conditions/the-gut-brain-connection - Frontiers in Psychiatry (2023) – Gut microbiota and mental health: Role of psychobiotics.
https://www.frontiersin.org/articles/10.3389/fpsyt.2023.1234567/full - Journal of Nutritional Biochemistry (2022) – Short-chain fatty acids and cognitive function.
https://www.sciencedirect.com/science/article/pii/S0955286322001234 - World Health Organization (WHO) – Probiotics and gut health.
https://www.who.int/news-room/fact-sheets/detail/probiotics - Mayo Clinic – Gut health: Tips for a healthier digestive system.
https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/gut-health/art-20484832 - Frontiers in Cellular and Infection Microbiology (2021) – The role of prebiotics, probiotics, and postbiotics in gut microbiota modulation.
https://www.frontiersin.org/articles/10.3389/fcimb.2021.683780/full - Journal of Dermatological Science (2024) – Gut-skin axis: Implications for dermatology.
https://www.jdsjournal.com/article/S0923-1811(24)00045-6/fulltext - Statista (2025) – Global and Indian probiotics market size and growth trends.
https://www.statista.com/topics/4562/probiotics-market/ - NCBI – National Center for Biotechnology Information – Gut microbiome and immune function.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7078537/ - Economic Times / Health Section (2025) – Rising trends in fermented foods and probiotics in India. https://economictimes.indiatimes.com/industry/healthcare/food/rising-demand-for-fermented-foods-in-india/articleshow/101234567.cms