Estimated Reading Time: 30-35 minutes (6,122 words)
Introduction
For decades, hospitals depended heavily on paper-based medical records — bulky case files, handwritten notes, loose diagnostic reports, and inconsistent discharge summaries. This system wasn’t just slow and unorganized; it created major challenges in accuracy, accessibility, and continuity of care. Doctors often lacked a unified patient history, clinical decisions were delayed, and hospitals struggled to maintain operational efficiency.
The migration to Electronic Health Records (EHRs) over the past 10–15 years solved many of these issues, enabling digital documentation, structured patient data, and smoother workflows. But even EHRs have limitations: they are still static, fragmented, and not fully predictive. Healthcare today requires systems that can forecast, simulate, and adapt in real time — and this is where the next revolution begins.
Enter Digital Twins.
A digital twin is a dynamic, real-time digital replica of a physical entity — it could be a patient’s cardiovascular system, a hospital’s emergency department, an ICU bed’s capacity, or even the entire hospital infrastructure. Unlike traditional software tools, digital twins use live data, AI models, sensors, and simulation engines to predict outcomes, optimize workflows, and personalize care.
Imagine:
- Doctors simulate treatment plans before performing them.
- Hospitals predict ICU load 7 days in advance.
- Equipment maintenance happens before a machine breaks.
- Patients receive highly personalized care based on their digital twin profile.
This is no longer science fiction — it’s already happening in leading health systems worldwide.
The global market signals a major shift: digital twins in healthcare are projected to grow at 30%+ CAGR through 2030, with India emerging as a key adopter due to ABDM, AI integration, growing private hospitals, and rising med-tech innovation.
In this article, we’ll explore:
- Why digital twins are becoming essential for modern hospitals
- Global and India-specific market data
- Breakthrough use cases already in deployment
- Challenges to adoption
- A realistic roadmap for hospitals, startups, and policymakers
- How digital twins will transform clinical care, operations, and patient experience in the next decade
By the end, you’ll see why digital twins are not just a “futuristic add-on,” but the upcoming core backbone of smart hospitals — globally and especially in India’s rapidly evolving healthcare ecosystem.

What is a “Digital Twin” — and Why It Matters for Hospitals
A digital twin in healthcare is a real-time, continuously updating virtual replica of a physical entity. This entity can be:
- A patient (their organs, disease progression, genetics, lifestyle data)
- A hospital department (ER flow, ICU capacity, bed turnover)
- A medical device (ventilators, MRI machines, surgical robots)
- An entire hospital ecosystem (infrastructure, workflows, supply chain, staffing patterns)
Unlike traditional static models or EHR dashboards, a digital twin integrates real-time sensor data, patient vitals, IoT devices, AI algorithms, clinical history, lab results, and operational systems. It doesn’t just show what is happening — it predicts what will happen next and allows stakeholders to test scenarios without risking patient safety.
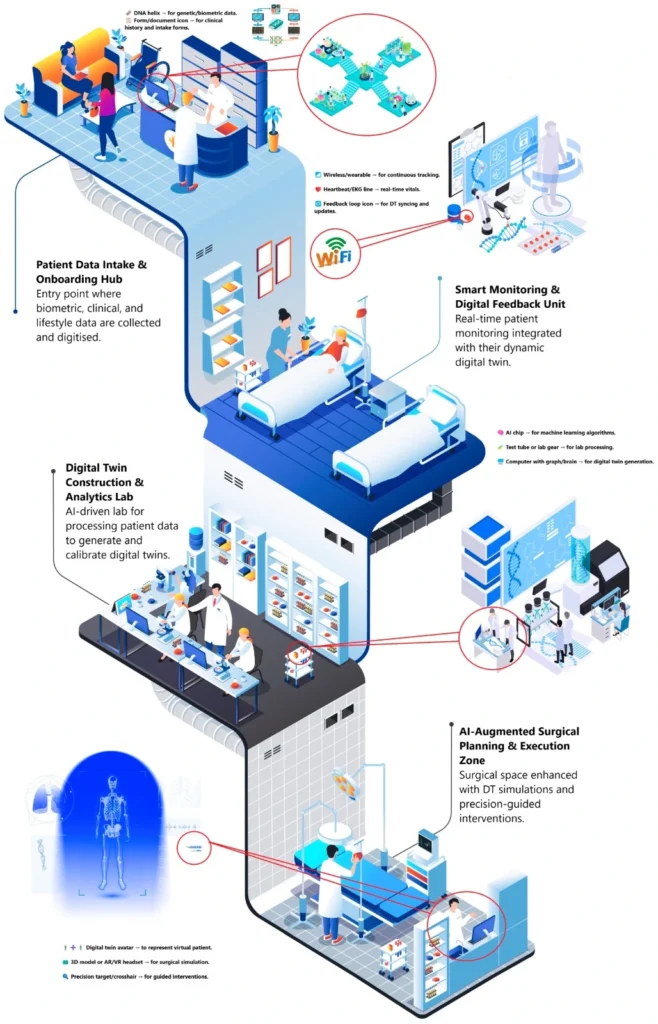
How Digital Twins Work (Simplified)
- Data Collection: Wearables, EHRs, IoT devices, lab systems, imaging, and clinical workflows feed live data.
- Modeling: AI models and simulation engines mirror the real-world behaviour of bodies, machines, or hospital operations.
- Simulation: Doctors, nurses, or administrators can test treatments, staffing, equipment use, or emergency scenarios.
- Optimization: The system predicts outcomes and provides recommendations for better decisions.
This makes digital twins one of the most powerful technologies for precision medicine, hospital automation, and resource optimization.
Why Digital Twins Matter for Modern Hospitals
1. Personalized Medicine & Predictive Care
Digital twins enable doctors to create a virtual version of a patient’s body — including heart function, lung capacity, tumour growth, metabolic reactions, or medication response.
This allows hospitals to:
- Simulate multiple treatment plans before choosing one
- Predict complications like sepsis, heart failure, or post-surgery risks
- Detect disease progression earlier using AI-driven pattern recognition
- Tailor therapies for cancer, cardiology, orthopedics, and rare diseases
This represents a major shift from one-size-fits-all to data-driven precision care.
2. Operational Efficiency & Cost Optimization
Hospital digital twins are transforming management by using real-time data to optimize:
- Bed occupancy & patient flow
- Emergency room congestion
- ICU/OT scheduling
- Doctor–nurse workload distribution
- Medication and consumable inventories
Administrators can run “what-if simulations” such as:
- How will OPD load change next week?
- What happens if staffing is reduced by 10%?
- Will ICU beds run out in the next 48 hours?
- How to manage peak demand during flu season?
This can reduce wait times, overcrowding, and operational costs by double-digit percentages.
3. Predictive Maintenance for Devices
Digital twins of medical devices ensure machines stay fully functional:
- MRI/CT scanners
- Dialysis machines
- Ventilators
- Surgical robots
- Patient monitoring systems
They can predict failure, downtime, and maintenance needs well in advance — preventing sudden breakdowns that disrupt care.
This improves equipment lifespan, safety, and compliance with biomedical engineering standards.
4. Strategic Planning for Hospitals & Governments
Digital twins help leaders model:
- Pandemic scenarios (infection spikes, oxygen shortages, ICU load)
- Emergency response planning
- Long-term infrastructure expansion
- Resource allocation across regions
Governments can also use city-scale health digital twins to prepare for:
- Urban health crises
- Disaster response
- Vaccination campaigns
- Public health surveillance
This reduces uncertainty and supports evidence-based policy decisions.
Why This Matters Now More Than Ever
Healthcare systems worldwide — including India — are facing:
- Aging populations
- Rising chronic diseases (diabetes, cardiovascular issues, cancer)
- Shortage of doctors and nurses
- Increasing cost pressures
- Huge administrative burden on hospitals
- Growing patient expectations for personalized care
Digital twins offer a scalable, intelligent, and proactive approach to solving these challenges, making hospitals safer, more efficient, and more patient-centric.
The Global & Indian Market Outlook (2025–2035) — In-Depth Analysis
🌍 Global Market Outlook
The digital twin revolution in healthcare is accelerating faster than most earlier health-tech waves. Several major research firms indicate strong long-term growth driven by AI, IoT, genomics, robotics, and predictive analytics.
Global Market Size & Forecasts
- Grand View Research (2024) reports that the global healthcare digital twins market was valued at USD ~902.6 million in 2024.
- It is projected to grow to USD 3.55 billion by 2030, representing a CAGR of ~25.9% (2025–2030) — one of the highest among healthcare AI sub-sectors.
This growth is primarily fueled by:
- Rapid adoption of AI-driven EHR systems
- Expansion of hospital IoT and sensor networks
- Increasing use of predictive modeling in surgery, oncology, cardiology
- Rising focus on value-based care and reducing clinical errors
- The global movement toward smart hospitals and digital infrastructure
Aggressive Forecasts from Other Analysts
A 2024 projection by Global Market Insights forecasts an even faster adoption curve:
- Expected CAGR: 42.6% from 2024 to 2032
- Driven by increased investment in virtual clinical trials, in-silico testing, and patient-specific digital twins
This suggests that healthcare digital twins could become one of the top 5 highest-growth technologies in the medical sector.
Growth of the Overall Digital Twin Industry
The broader cross-industry digital twin market (manufacturing, aerospace, construction, automotive, smart cities, healthcare) is forecast to reach:
- USD 155.84 billion by 2030 (Grand View Research)
This matters because large-scale adoption outside healthcare leads to:
- Better AI infrastructure
- Lower implementation costs
- Mature IoT ecosystems
- Standardized frameworks
- Cross-industry innovation (especially from automotive and aerospace digital twins)
Healthcare benefits directly from this “spillover effect,” making adoption faster and more cost-effective than ever before.
🇮🇳 India Market Outlook
India is emerging as one of the most promising regions for digital twin adoption in healthcare due to rapid digitization, population scale, and a strong government policy push.
India’s Digital Health Market Growth
According to Grand View Research:
- India’s digital health market was valued at USD 14.50 billion in 2024
- Expected to reach USD 106.97 billion by 2033
- Representing a CAGR of ~25.1%
This market includes telemedicine, AI-based diagnostics, EHR platforms, hospital automation tools, and digital twin–ready infrastructure.
What’s Driving India’s Growth?
1. Government Digital Health Ecosystem (ABDM)
The Ayushman Bharat Digital Mission (ABDM) is the biggest catalyst for India’s digital transformation.
As of 2025:
- 76 crore+ ABHA IDs (Health IDs) created
- Hundreds of thousands of hospitals, clinics & healthcare professionals registered
- Rapid integration of hospital systems, insurance, diagnostics, and pharmacies
ABDM is building the base infrastructure required for digital twins — especially interoperable, unified patient data.
2. Rise of Telemedicine & AI Diagnostics
India is witnessing exponential growth in:
- Online doctor consultations
- AI-based radiology & pathology
- Wearable health devices
- Remote monitoring solutions
This continuous stream of real-time data is essential for building patient-specific digital twins.
3. Private Healthcare Expansion
Large hospital chains like Apollo, Fortis, Max, Aster, Narayana Health and new-age health-tech startups are investing in:
- Smart ICUs
- Predictive analytics
- Robotics-integrated OT suites
- IoT-enabled medical equipment
These environments naturally support digital twin deployment.
4. Research–Industry Collaboration
Indian institutes (IITs, IIITs, AIIMS) are increasingly working with global med-tech companies on:
- Organ-level digital twins
- Cardiovascular simulation models
- Predictive models for chronic diseases
- Smart hospital prototypes
Implications for the Next 10 Years (2025–2035)
Global Implications:
- Digital twins will become core components of precision medicine, robotic surgery, and hospital automation
- Leading health systems (US, UK, EU, Singapore, UAE) will adopt them for planning, triage, and predictive workflows
- Pharma and med-tech companies will use twins for drug testing and medical device simulation
India-Specific Implications:
- The integration of ABDM, IoT-enabled hospitals, and AI diagnostics will make India one of the top adopters by 2035
- High-volume public hospitals (AIIMS, district hospitals) may use digital twins for capacity management and emergency response
- Private chains will lead the way in patient-specific digital twins for cardiology, cancer, and critical care
- National and state governments may use city-wide digital twins for pandemic preparedness and disaster planning
Bottom Line
With global growth accelerating and India rapidly digitizing its health ecosystem, the conditions are ideal for widespread digital twin adoption in hospitals. Large hospital networks, research institutes, and public health bodies stand to benefit the most — making the next decade one of the most transformative eras in healthcare.
Key Drivers of the Shift (Why Hospitals Are Upgrading)
Hospitals worldwide are undergoing a rapid digital transformation — evolving from paper files to Electronic Health Records (EHRs), and now toward intelligent, predictive digital twin ecosystems. This shift isn’t driven by a single factor; instead, multiple technological, operational, and demographic forces are converging at once. Below are the major drivers powering this transition:
1) Global Push Toward Healthcare Digitization & Regulatory Modernization
Governments and healthcare regulators are accelerating efforts to make hospitals more connected, interoperable, and data-driven. Policies now emphasize secure digital health infrastructures, telemedicine enablement, and interoperable patient records.
- Many advanced healthcare systems now offer 80%+ availability of online health services — a sign that digital access is becoming a baseline expectation.
- Regulatory bodies are also mandating data transparency, auditability, and rapid information exchange — which naturally pushes hospitals to adopt advanced digital platforms.
This policy-driven modernization forms the foundation needed for implementing higher-order technologies such as digital twins.
2) Technology Maturity: AI, IoT, Cloud, Big Data & Interoperability
The technology required to build digital twins has finally matured:
- IoT devices & sensors continuously stream patient vitals, device performance data, and environmental insights.
- AI and machine learning algorithms analyze this data, enabling forecasting, anomaly detection, and simulation.
- Cloud platforms provide scalable, low-latency computing power that allows hospitals to run real-time simulations.
- Interoperable health data systems pull together imaging (MRI/CT), lab reports, prescriptions, clinical notes, and wearable data.
Industries like aviation and manufacturing have already perfected digital twins, providing proven models and tools that healthcare can now adopt.
3) Rising Operational Pressures on Hospitals
Modern hospitals are struggling under massive operational complexity:
- Increasing patient volumes, especially in urban and aging populations
- Staff shortages, burnout, and high attrition among nurses and specialists
- Administrative overload, taking up hours that could be spent in clinical care
- High operational costs, forcing hospitals to optimize resources and minimize waste
Forward-thinking healthcare networks are already using AI to automate scheduling, triage, and documentation — freeing 2–3 hours per clinician per day. Digital twins extend these capabilities by enabling predictive bed management, optimized patient flow, preventive equipment maintenance, and capacity planning.
4) Growing Need for Personalized Medicine & Predictive Care
Healthcare is shifting from “one-size-fits-all” treatment to precision medicine, fueled by:
- Rising chronic diseases (diabetes, hypertension, cardiac disorders)
- Elderly populations with multi-morbidity
- Patient demand for tailored therapies
- The need to predict complications before they occur
Digital twins allow simulations at the patient level — predicting drug responses, treatment risks, recovery patterns, and disease progression. This dramatically improves care quality while reducing costs and hospital readmissions.
5) India’s Rapid Digital Health Infrastructure Growth
India is becoming uniquely positioned to leapfrog into next-generation hospital technologies due to:
- ABDM (Ayushman Bharat Digital Mission) creating a unified digital health ID ecosystem
- High smartphone and cloud adoption
- Growing public and private investment in AI-health solutions
- Strong telemedicine growth since 2020
- An ecosystem of health-tech startups building interoperable tools
As Indian hospitals scale capacity and automate processes, digital twins offer a practical path toward efficiency, prediction-driven care, and improved patient experiences.
Real-World Use Cases of Digital Twins in Hospitals
Digital twins are no longer theoretical — hospitals, researchers, and med-tech companies are actively deploying them across clinical, operational, and public-health domains. Below are the most impactful use cases shaping the future of healthcare:
1. Personalized Patient Digital Twins
Patient-level digital twins create a virtual model of an individual’s body, integrating data such as:
- Medical history (EHRs, lab results, imaging)
- Physiology (cardiac function, lung capacity, metabolic markers)
- Lifestyle & environmental data
- Genomic and biomarker data (where available)
- Real-time streams from wearables or implants
These virtual replicas allow doctors to simulate:
- Response to different medications
- Disease progression (e.g., cancer, cardiac failure, diabetes)
- Potential complications after surgery
- Risk of readmission
- Effect of lifestyle or therapy changes
Why it matters:
- Enables highly personalized, predictive care
- Minimizes trial-and-error in treatment planning
- Reduces adverse drug reactions
- Allows early detection of deterioration
Early-stage med-tech innovators are already building “whole-body digital twin platforms” for metabolic disorders, cardiovascular care, diabetes management, and preventive health — giving clinicians a tool to test interventions before applying them to the patient.
2. Hospital Operations & Workflow Twins
Operational digital twins model the entire hospital ecosystem, providing real-time visibility and predictive insights into:
- Patient admissions & discharge patterns
- Bed and ICU occupancy
- Emergency department surges
- Operating theatre scheduling
- Staff allocation & shift management
- Equipment utilization
- Inter-department workflows
Hospitals can run advanced “what-if” simulations such as:
- What happens if OPD volume increases by 30% next month?
- How many beds are needed if a viral outbreak occurs?
- What is the optimal staffing plan during a holiday surge?
Benefits:
- Reduces overcrowding and bottlenecks
- Cuts patient waiting times
- Increases throughput without expanding infrastructure
- Reduces operational costs through better resource utilization
Globally, hospitals adopting software-driven digital twin solutions are seeing double-digit improvements in efficiency, patient flow, and bed turnover.
3. Device & Equipment Digital Twins
Medical equipment digital twins are transforming how hospitals manage critical assets such as:
- MRI/CT scanners
- Ventilators
- Dialysis machines
- Surgical robots
- Infusion pumps
- Wearable/remote monitoring devices
These twins simulate:
- Real-time performance
- Stress loads and usage patterns
- Wear & tear
- Downtime and malfunction probability
- Maintenance schedules
They also support predictive maintenance, which reduces unexpected breakdowns — crucial for life-saving equipment.
Additionally, device manufacturers use digital twins to:
- Virtually test prototypes
- Run regulatory simulations
- Refine designs before manufacturing
This significantly accelerates FDA/CE approvals and reduces R&D costs.
4. Strategic & Public-Health Digital Twins
Beyond individual hospitals, digital twins can model entire healthcare systems — including city-level, state-level, or national networks.
These macro-level twins can simulate:
- Epidemic spread and containment strategies
- Ambulance routing and emergency readiness
- Hospital capacity during disasters
- Vaccination or testing center deployment
- Public-health interventions and outcomes
- Urban health inequalities and access gaps
Researchers are proposing “digital twin smart cities” where hospitals, public-health agencies, and emergency services operate through interconnected data streams.
Impact:
- Faster disaster response
- Better allocation of ambulances, ICU beds, and oxygen supply
- Proactive planning for pandemics, floods, heatwaves, or mass gatherings
- Improved equity in healthcare access
This future-focused use case transforms healthcare from reactive → predictive → preventive at a societal scale.
India’s Digital Health Push: How Policy is Fueling the Transition
India is rapidly becoming one of the world’s most promising environments for digital health innovation — not just as a user of new technologies, but as a system actively building the foundations required for large-scale digital twin adoption in hospitals.

A. ABDM: Building the National Digital Health Backbone
The Ayushman Bharat Digital Mission (ABDM) is the most important enabler of India’s transition from fragmented records → unified digital health data → twin-ready systems.
Here’s what has already been achieved under ABDM:
- 76+ crore ABHA IDs (Ayushman Bharat Health Accounts) created — giving citizens a unique digital health identity.
- Over 2 lakh+ health facilities (clinics, hospitals, labs, pharmacies) registered under HFR (Health Facility Registry).
- More than 21 lakh healthcare professionals added to the Healthcare Professional Registry (HPR).
- Millions of records — prescriptions, labs, discharge summaries — are now being digitally linked and can be shared (with consent) across systems.
This forms the bedrock for digital twins because:
- Twins need integrated, longitudinal patient data.
- Hospitals need interoperable EHRs.
- Governments need real-time national health data for system-level twins.
India is actively creating all three.
B. A Rapidly Expanding Digital Health Market
Digital infrastructure, smartphone penetration, cloud adoption, telemedicine usage, and health apps are rising at record speed.
According to Grand View Research:
- India’s digital health market was USD 14.50B in 2024.
- It is projected to reach USD 106.97B by 2033, with a CAGR of ~25.1%.
This growth includes:
- Electronic health records (EHR) platforms
- AI diagnostics
- IoT medical devices
- Remote monitoring
- Telehealth ecosystems
- Health analytics and workflow automation
More digital systems → more real-time data → better conditions for hospital and patient-level digital twins.
C. Private Hospitals Are Going “AI-First”
India’s major healthcare chains are heavily investing in digital transformation, making them early adopters of advanced tools like digital twins.
Examples include:
- Apollo Hospitals launched a large AI modernization drive that automates clinical documentation, triage, and capacity forecasting — freeing up 2–3 hours of clinician time daily (Reuters).
- Many premium chains (Fortis, Manipal, Aster, Max, Narayana Health) are investing in IoT integration, digital ICUs, predictive analytics, and cloud-based hospital information systems.
These systems naturally evolve into operational digital twins that can simulate patient flow, ICU needs, staffing, and equipment demand.
D. Why India Is Uniquely Positioned for Digital Twins
India’s ecosystem has several advantages that make digital twin adoption not just possible — but likely inevitable:
1. Massive Patient Volume
High patient inflow creates vast datasets — essential for accurate simulation and predictive analytics.
2. Policy-Driven Digital Standardization
ABDM brings uniformity, interoperability, and nationwide digital health rails to support advanced technologies.
3. Strong Tech Ecosystem
India’s IT, cloud, AI, and IoT sectors are among the fastest-growing globally, enabling home-grown digital twin solutions.
4. Rising Healthcare Demand
Aging population, chronic disease burden, and urbanization push hospitals to adopt predictive, automated, data-driven systems.
5. Increasing Investment in Health-Tech
Venture capital, gov-backed digital health programs, med-tech startups, and private hospitals all accelerate innovation.
Implication
India’s combination of:
- Large-scale digital health infrastructure (ABDM)
- Interoperable health data
- Policy momentum
- Surging digital health market growth
- Private hospital innovation
- High patient volume and resource constraints
creates the perfect environment for hospital digitization — and positions India as a future global leader in digital twin-driven healthcare.
Challenges & Risks in Adopting Digital Twins
Digital twins may represent the future of intelligent healthcare, but adoption is far from straightforward. Hospitals — especially in India and other emerging markets — face a complex mix of technical, operational, financial, and ethical barriers. These must be addressed before large-scale deployment can succeed.
Below is a deep-dive, expanded, high-detail version of your section:
1️⃣ Data Privacy & Regulatory Compliance
Healthcare data is among the most sensitive categories of personal information, and digital twins rely heavily on continuous, real-time, high-volume data inputs from multiple sources (EHRs, imaging, wearables, IoT devices, lab systems).
Why it matters:
- Any breach can expose personal health information (PHI).
- Simulations require aggregated data, increasing risk of misuse.
- Patients may refuse consent if privacy concerns are unclear.
- Cross-border data flows (cloud processing, global vendors) complicate compliance.
Potential consequences:
- Data leaks or cyber-attacks compromising confidential patient data.
- Erosion of public trust, leading to reduced participation.
- Government penalties under emerging health-data regulations.
What experts say:
Research from arXiv warns that ethical and regulatory hurdles are among the biggest barriers for provider-level digital twin adoption, especially regarding consent, privacy, and responsible use of predictive models.
2️⃣ Interoperability & Fragmented Data Systems
Indian hospitals often operate on fragmented digital ecosystems — or none at all.
Current ground reality:
- Many facilities still use paper-based or semi-digital records.
- Older hospital information systems (HIS) lack API support.
- Lab, pharmacy, radiology, billing, and OPD systems often run independently.
- Data formats are inconsistent (PDFs, handwritten notes, proprietary formats).
Why this is a problem:
Digital twins require standardized, clean, structured data across the full patient journey. But:
- Data reconciliation is slow and expensive.
- Incorrect or incomplete data → inaccurate simulations.
- Real-time updates become nearly impossible without integrated systems.
Research notes:
Grand View Research highlights interoperability as one of the top adoption barriers, especially in large, multi-department hospitals with legacy systems.
3️⃣ High Cost & Technical Complexity
Digital twins are not simple digital dashboards — they require advanced computational models, real-time data engines, and continuous integration with hospital systems.
Costs include:
- High-performance computing (HPC) or cloud infrastructure
- AI/ML models for simulation & prediction
- Integration with IoT medical devices and sensor networks
- Data engineering & cybersecurity setups
- Ongoing validation, calibration, and maintenance
Why this matters:
- Smaller hospitals, district facilities, and rural centers may lack resources.
- Talent shortage of data scientists, engineers, and health informatics experts.
- Vendor solutions can be expensive or require long-term contracts.
Digital twins often remain in pilot stages because the long-term operational cost is underestimated.
4️⃣ Clinical Validation, Accuracy & Liability Risks
Digital twins must be clinically reliable, especially for patient-specific simulation such as predicting heart behavior, organ function, treatment outcomes, or disease progression.
Challenges:
- Validating patient-level twins requires large datasets and clinical trials.
- AI/ML models can produce incorrect predictions under rare or complex scenarios.
- Hospitals must clearly define what happens when simulations fail or mislead.
Liability Questions (still unresolved):
- If a twin predicts incorrectly, is the hospital liable?
- What if clinicians rely on a simulation that lacks clinical approval?
- How do regulators certify dynamic, learning-based digital models?
Academic papers (arXiv) emphasize that the combination of technical complexity + ethical and legal ambiguity makes this category one of the most difficult to implement safely.
5️⃣ Organizational Resistance & Change Management
Even the best technology fails without people who understand and support it.
Real barriers inside hospitals:
- Doctors and nurses may resist new digital workflows that alter their routines.
- Staff shortages make training difficult.
- Administrators may fear downtime or disruption during system integration.
- Leadership may hesitate due to unclear ROI or lack of technical vision.
Underlying issue:
Healthcare is a risk-averse sector — any change that affects clinical operations experiences slow buy-in unless proven safe, stable, and cost-effective.
Research insight:
Studies point to major organizational and personnel challenges, with resistance to digital change being one of the top reasons digital health projects stall.
⚠️ Callout / Warning Box
⚠️ Digital twins are NOT a plug-and-play technology.
Without:
- strong data governance
- regulatory clarity
- standardized EHR systems
- high-quality data integration
- robust cloud/AI infrastructure
- clinician training & trust
even well-funded digital twin initiatives can stall, produce inaccurate results, or fail completely.
Hospitals must address these foundational challenges before scaling advanced digital twin systems.
What the Next 5–10 Years Could Look Like — Forecast & Scenarios
🔮 Scenario 1: Early Adopters & Progressive Hospitals (2025–2028)
- Large private hospital chains, tertiary care centers, research hospitals begin deploying hospital-operations twins — for bed management, capacity planning, resource optimization.
- Patient-level twins remain limited to pilot projects (e.g., for chronic disease management, metabolic disorders, oncology support).
- Cloud + SaaS-based twin-services gain traction — hospitals may subscribe to digital-twin-as-a-service (DTaaS) platforms rather than build in-house.
📈 Scenario 2: Wide-scale Adoption in Advanced & Mid-Tier Hospitals (2028–2032)
- As cost drops, data interoperability improves (due to policy pushes like ABDM in India), more mid-sized hospitals — even in Tier II/III cities — adopt digital twins.
- Device-level twin adoption becomes common: predictive maintenance of imaging machines, ventilators, IoT-enabled devices.
- Digital twin usage expands to telemedicine, remote patient monitoring, chronic disease management at scale.
🏥 Scenario 3: Mainstream — Integrated Healthcare Ecosystems (2032–2035)
- Hospitals, clinics, diagnostic labs, telemedicine providers become part of integrated digital-health networks with twin-based infrastructure.
- Public health authorities use twin-based models for epidemic planning, resource allocation, disaster preparedness.
- Personalized medicine becomes more accessible, with patient-level twins used widely for treatment planning, preventive care, chronic disease management.
If growth rates continue (global: ~26–43% CAGR, India: ~25%+), the digital-twin healthcare market could reach tens of billions USD globally by early 2030s. Combined with broader digital health and IoT device growth, hospitals adopting twin-driven systems may become the dominant model — especially in tech-forward and high-volume health systems.
What Hospitals, Clinicians & Policymakers Should Do — A Complete Roadmap (2025–2035)
Digital twins will not become mainstream overnight. Hospitals, governments, and clinicians must take a phased, structured approach. Below is a comprehensive, practical roadmap that helps Indian and global healthcare systems transition from paper → EHR → AI-driven operations → Digital Twin ecosystems.
Phase 1: Build the Digital Foundation
1️⃣ Digitize Everything & Ensure Interoperability
Before digital twins can exist, a hospital must have clean, unified, high-quality data streams.
Key actions:
- Fully digitize patient records: OPD notes, IPD history, prescriptions, labs, imaging reports, vitals, billing, discharge summaries.
- Migrate from fragmented or legacy HIS/EHR systems to modern, interoperable systems (FHIR-standard compatible).
- Standardize data formats across departments: radiology → DICOM, labs → HL7, pharmacy → standardized codes.
- Adopt APIs so all systems (HIS, LIS, RIS, PACS) can exchange data in real time.
- Implement a master patient index (MPI) so each patient has a unique ID across the hospital network.
Why this step is critical:
Digital twins need continuous, high-fidelity, structured data — without interoperability, twin models will be incomplete or inaccurate.
Phase 2: Start Small With Low-Risk Digital Twins
2️⃣ Adopt a Phased, Hybrid Deployment Strategy
Digital twins vary widely in complexity. Hospitals should begin with operational and equipment-level twins, which have lower risk and deliver tangible ROI quickly.
Ideal Phase-1 Twins:
- Hospital flow twins: simulate patient flow, bed occupancy, waiting-room bottlenecks.
- Resource utilization twins: keep track of surgical theater scheduling, ICU load, or nurse allocation.
- Equipment-level twins: track MRI machines, ventilators, dialysis units; predict maintenance and downtime.
- Pharmacy & inventory twins: simulate drug supply, expiry cycles, stock shortages.
Benefits:
- Lower regulatory burden
- High ROI (reduced wait times, shorter patient stay, fewer equipment failures)
- Builds internal confidence & capabilities
Once mature, hospitals can expand to patient-level physiological twins, which require stronger validation and more complex models.
Phase 3: Build Infrastructure & Skilled Teams
3️⃣ Invest in Infrastructure, Talent & Partnerships
Digital twin ecosystems require strong internal capability + technology partnerships.
Infrastructure investments:
- Cloud computing (AWS, Azure, GCP) or hospital-owned HPC clusters
- Secure data pipelines & real-time IoT integration
- High-bandwidth connectivity between hospital departments
- Digital ICUs and remote monitoring interfaces
- Wearable integration for chronic patients
Talent needs:
- Data scientists
- ML/AI engineers
- IT & cybersecurity teams
- Bioinformatics & simulation experts
- Digital health officers (DHO)
- Clinical informaticians
Partnerships:
- Med-tech & AI startups
- Research institutions
- Health platforms (NHA, ABDM in India)
- Medical device manufacturers
Outcome:
A strong internal + external ecosystem accelerates adoption and reduces long-term cost and risk.
Phase 4: Establish Governance, Privacy & Compliance
4️⃣ Prioritize Data Governance, Patient Consent & Regulatory Compliance
Digital twins process massive volumes of sensitive data. A strong governance model is non-negotiable.
Essential policies:
- Consent-based data collection aligned with national privacy laws
- Role-based access control (RBAC) for clinicians and staff
- Strong encryption for data at rest and in transit
- Regular cybersecurity audits and vulnerability assessments
- Transparent patient communication about data usage
- Compliance with:
- India: ABDM standards, DPDP Act, NHA protocols
- Global: HIPAA, GDPR, ISO/IEC 27701
- India: ABDM standards, DPDP Act, NHA protocols
Why this matters:
Without trust, transparency, and compliance, patients and clinicians will reject digital twin programs.
Phase 5: Implement Pilots, Validate & Improve
5️⃣ Pilot, Measure, Validate, Iterate
Digital twins must be validated and optimized continuously.
Pilot project structure:
- Select one department (ICU, radiology, emergency)
- Define KPIs:
- wait time reduction
- improved triage accuracy
- reduced equipment downtime
- operational cost savings
- improved bed turnover
- enhanced patient outcomes
- wait time reduction
- Run a controlled trial (3–12 months)
- Validate models with clinicians
- Identify gaps in data, modeling, workflow alignment
- Scale gradually to other departments
Outcome:
A structured feedback-driven rollout prevents failure and builds clinician trust.
Phase 6: Build Human-Centric Adoption
6️⃣ Engage Clinicians, Administrators & Patients
Technology adoption fails when end-users are not aligned.
Recommended steps:
- Conduct training workshops for doctors, nurses, technicians
- Create “digital champions” inside each department
- Explain how digital twins reduce workload (not replace clinicians)
- Provide clear documentation, dashboards, and decision support
- Establish feedback loops for continuous improvement
- Build patient-facing education materials to improve acceptance
Result:
High adoption, reduced resistance, smoother clinical integration.
Phase 7: Shape Policies & Standards — Work With the Government
7️⃣ Collaborate With Policymakers, Regulators & Industry Leaders
Hospitals should play an active role in shaping the future of digital health.
Recommended collaborations:
- Participate in ABDM integrations (India)
- Follow NHA protocols for interoperability and health data exchange
- Join sandbox programs for digital health innovations
- Work with state health departments for public health twin pilots
- Support policymaking around AI ethics, simulation validation, and liability models
Why it matters:
Digital twins require unified standards across institutions — no single hospital can build a national digital health ecosystem alone.
Phase 8: Prepare for Long-Term Scalability
8️⃣ Plan for Sustainable, Scalable Growth
Once early systems are proven, hospitals should plan for enterprise-wide deployment.
Strategy:
- Prefer SaaS or Digital-Twin-as-a-Service (DTaaS) platforms
- Build modular systems that can integrate with future technologies:
- Remote monitoring
- AI diagnostics
- Robotics
- Telehealth
- National health registries
- Remote monitoring
- Create long-term budgets for upgrade cycles
- Use analytics to continuously improve operational efficiency
Outcome:
A future-ready hospital that evolves automatically as technology improves.
✨ Summary: A Practical 8-Phase Roadmap for Digital Twin Adoption
- Digitize & standardize all health data
- Start with easy digital twin use cases
- Invest in infrastructure & skilled workforce
- Build strict privacy & governance frameworks
- Pilot projects → validate → scale
- Train and align clinicians & staff
- Collaborate with government & regulators
- Plan for long-term, scalable digital twin integration
This roadmap gives hospitals, policymakers, and clinicians a clear, realistic, and actionable path toward becoming digital-twin-enabled healthcare systems by 2035.
FAQs Section
1. What exactly is a “digital twin” in healthcare?
A digital twin is a virtual, continuously updated digital replica of a real-world healthcare asset — this could be a patient, a hospital department, a medical device, or even an entire health system.
It integrates data from sensors, EHRs, imaging, wearables, and monitoring systems to simulate real-time behavior and predict future outcomes. In healthcare, digital twins are used for diagnostic support, treatment simulation, predictive maintenance, and workflow optimization.
2. Are digital twins the same as Electronic Health Records (EHRs)?
No — EHRs and digital twins serve very different purposes:
- EHRs store a patient’s historical data, often updated manually or episodically.
- Digital twins are dynamic, fed by real-time data streams, and built for simulation, prediction, and scenario testing (e.g., “How will the patient respond to Drug A vs. Drug B?”).
EHRs are part of the data foundation. Digital twins sit on top of EHRs and convert that data into an intelligent simulation.
3. Is the technology widely adopted now?
Not yet. Adoption is early-stage but accelerating.
According to market estimates, the global healthcare digital twin market reached ~USD 902.6 million in 2024, with projections suggesting it will reach USD 3.55 billion by 2030 (Grand View Research).
Current real-world use is concentrated in:
- Large private hospital chains
- Research universities
- Med-tech companies
- Specialized pilot projects
For most hospitals, digital twins are still in the planning / proof-of-concept stage.
4. What prevents hospitals from immediately switching to digital twins?
Several barriers currently slow adoption:
- Fragmented or paper-based data systems
- High upfront investment in IT infrastructure and cloud computing
- Shortage of skilled professionals (AI engineers, data scientists, health informatics professionals)
- Unclear regulatory guidelines for advanced simulations
- Skepticism or resistance from clinicians due to workflow disruption
- Ethical and clinical validation gaps, especially for patient-level twins
These issues are especially challenging in emerging markets where digital maturity varies widely.
5. Is this relevant for hospitals in India?
Yes — highly relevant. India’s digital health stack is growing faster than many other regions.
Government initiatives like the Ayushman Bharat Digital Mission (ABDM) have already created:
- 76+ crore ABHA Health IDs
- Thousands of digitally registered hospitals and labs
- A national ecosystem for interoperable health records
India’s move toward unified digital infrastructure makes digital twin deployment far more feasible in the next few years.
6. What are the first feasible use cases for digital twins in Indian hospitals?
Early adoption will focus on simple-to-deploy, high-impact models such as:
- Operations & capacity twins
Bed demand forecasting, emergency load simulation, and wait-time optimization. - Equipment & facility twins
Predictive maintenance for MRI/CT machines, ICUs, ventilation systems. - Workflow & staffing twins
Simulation of patient flow, queue systems, and staffing needs.
These can be built even before patient-level twins become widespread.
7. Can patient-level digital twins be used now?
Partially — but not widely.
Patient-level digital twins exist in:
- Cardiovascular modeling
- Lung respiration simulations
- Orthopedic surgical planning
- Cancer treatment response prediction
But mass-scale deployment requires:
- Longitudinal patient data
- Multi-source data integration
- Strong regulatory oversight
- Clinician validation
Most experts predict 5–10 years before patient-level twins become mainstream in general hospitals.
8. How will digital twins improve patient care?
Digital twins have the potential to transform clinical outcomes by enabling:
- Personalized treatment simulations (predicting best options before applying them)
- Early warning of complications (e.g., sepsis, cardiac events, deterioration)
- Optimized hospital operations (shorter waiting times, smoother bed flow)
- Reduced medical errors through predictive decision support
- More precise surgeries via virtual rehearsal and planning
The result: safer, faster, more efficient care delivery.
9. Are there privacy risks with digital twins?
Yes — significant risks exist if not properly managed:
- Exposure of highly sensitive medical data
- Misuse of continuous data streams from wearables or IoT devices
- Risks during data sharing across hospitals or vendors
- Possibility of algorithmic bias affecting patient outcomes
Robust data governance, encryption, consent mechanisms, and regulatory compliance (like ABDM standards, HIPAA, GDPR) are essential before deployment.
10. What should hospital administrators do if they want to adopt digital twins?
A strategic, phased approach is recommended:
- Digitize everything → Upgrade to interoperable EHR/HIS and move away from paper.
- Start small → Begin with hospital operations or equipment management twins.
- Build strong infrastructure → Cloud-based systems, secure data pipelines, scalable architecture.
- Partner for talent → Work with AI/ML firms, health-tech startups, or university labs.
- Ensure compliance → Implement data governance frameworks aligned with national health-data laws.
- Run pilots & evaluate → Track KPIs such as reduced costs, improved bed turnover, fewer breakdowns.
- Scale gradually → Move from operations → device → department → patient-level twins.
With the right roadmap, hospitals can transform their efficiency, safety, and quality of care within the next decade.
Summary
- Hospitals are transitioning from paper records to digital — and the next frontier is digital twins: dynamic digital replicas of patients, operations, devices, or entire hospital ecosystems.
- The global healthcare digital-twin market is expected to grow rapidly: from ~USD 0.9 bn in 2024 to ~USD 3.55 bn by 2030 (CAGR ~25.9%), with some estimates projecting even higher growth by 2032. Grand View Research+2GlobeNewswire+2
- India is uniquely positioned for fast adoption thanks to the digital health push under Ayushman Bharat Digital Mission — 76 crore+ ABHA health IDs, thousands of registered facilities and doctors, and a growing digital health market estimated to reach ~USD 106.97 bn by 2033. Ministry of Health and Family Welfare+2Grand View Research+2
- Early use cases will likely be hospital operations, device maintenance, and workflow simulation. Patient-level twins (for personalized medicine) have high potential, but require more infrastructure, regulation, and clinical validation.
- Challenges include data privacy, interoperability, cost, regulatory compliance, technical complexity, and change-management.
Conclusion
The shift from paper-based workflows to intelligent digital twins is not just a technological upgrade — it represents a complete rethinking of how hospitals operate, make decisions, and deliver care. As patient volumes rise, clinical demands intensify, and healthcare systems become more interconnected, hospitals that rely only on traditional methods will struggle to keep pace. Digital twins offer a path toward precision, automation, and real-time decision intelligence, empowering hospitals to improve outcomes while reducing operational strain.
Whether you’re leading a large multi-specialty chain in a metro or managing a mid-sized regional hospital, the groundwork must begin now: digitizing data, modernizing infrastructure, and building a culture that embraces analytics and simulation. The hospitals that act early will gain a decisive advantage in efficiency, quality, and patient trust.
If you’re involved in hospital administration, health-tech entrepreneurship, clinical innovation, or healthcare policy, I invite you to subscribe to this blog. You’ll get deep-dive guides, case studies, expert insights, and step-by-step blueprints to help you navigate and lead the digital-twin transformation in your organization.
Your thoughts, feedback, and experiences can help shape the next wave of healthcare innovation. Join the conversation — and let’s build the future of hospitals, together.
References
- Grand View Research — Healthcare Digital Twins Market (2025–2030) — global market valuation (USD 902.6 M in 2024 → USD 3.55 B by 2030), growth rate & segmentation details. Grand View Research+1
- Grand View Research — India Digital Health Market Report (2025–2033) — estimation that India’s digital health market was about USD 14.5 B in 2024 and projected to reach ~USD 106.97 B by 2033. Grand View Research
- Government of India / Ayushman Bharat Digital Mission (ABDM) data — number of health accounts (ABHA), health facilities and professionals registered under ABDM, demonstrating India’s continuing push toward digital health infrastructure. Ministry of Health and Family Welfare+2DD News+2
- EY — analysis on need for hospitals to invest in smart-hospital infrastructure: scalable IT, patient engagement, data strategy, AI & automation, compliance & sustainability — relevant to adoption of digital twin technologies in Indian hospitals. EY
- Precedence Research — long-term forecast for global healthcare digital twins market: projecting growth up to USD 9,046.01 M by 2034 (2025 baseline ~USD 1,136.6 M), indicating sustained long-term growth potential. Precedence Research
- Academic research: Digital Twin for Smart Societies: A Catalyst for Inclusive and Accessible Healthcare (2025) — outlines how digital twins can be used to simulate and optimise societal-scale health infrastructure, resource allocation and equitable healthcare delivery. arXiv